- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
CBT response in pediatric OCD may be predicted by MRI, reports study
A comparative study published in Journal of child psychology and psychiatry, conducted by David Pagliaccia et al and published in a recent edition of Journal of Child Psychology and Psychiatry revealed significant changes in structural and diffusion MRI which may be useful indicators in identifying pediatric patients who are expected to respond best to individual Cognitive behavioral therapy (CBT).
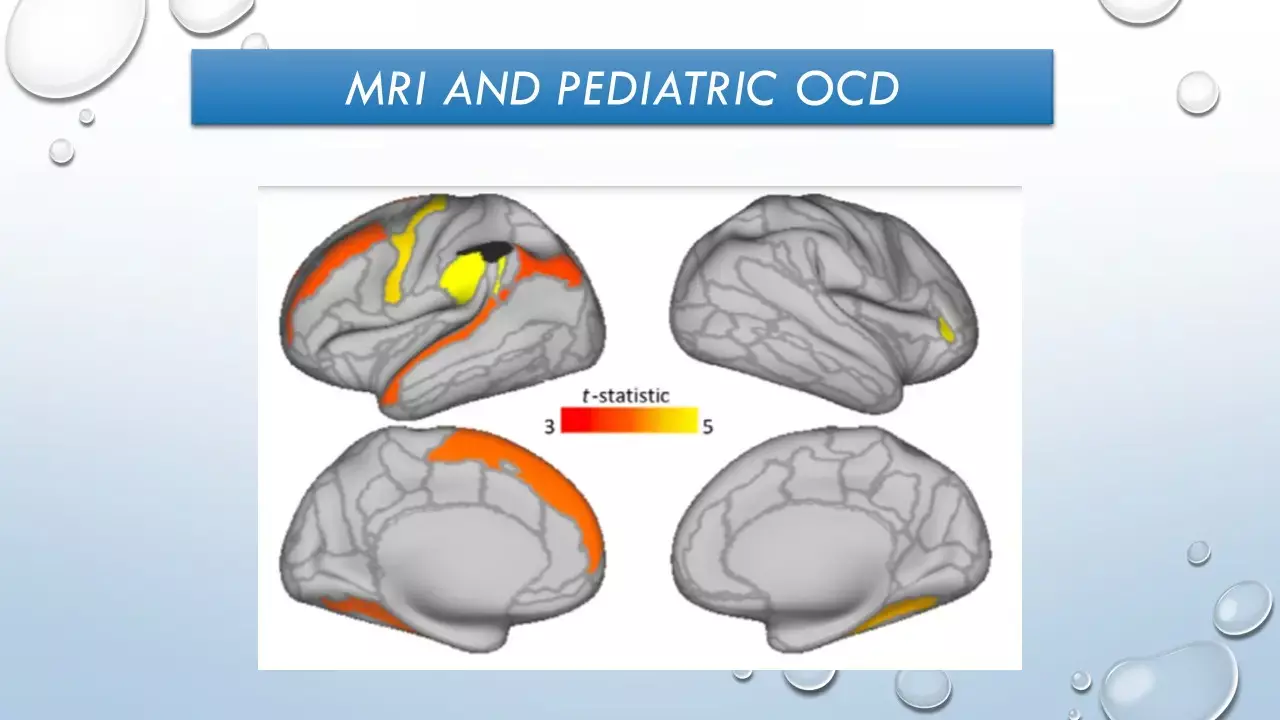
CBT is an effective, first-line treatment for pediatric obsessive-compulsive disorder (OCD). CBT with exposure and ritual prevention (EX/RP) is a first-line treatment for OCD. Earlier, functional MRI (fMRI) findings suggested functional alterations in frontoparietal and cingulo-opercular circuits in adults and youth with OCD during cognitive control paradigms. The functioning of these circuits is likely critical for engagement of control over obsessions and compulsions and, presumably, success abstaining from performing rituals during exposure-based CBT.
In this study, the authors investigated alterations in brain structure and structural connectivity in unmedicated children/adolescents with OCD and tested whether these structural measures predicted CBT outcomes. High-resolution structural and diffusion-weighted MRI data were acquired before patients completed 12–16 CBT sessions. It was hypothesized that:
(a) Variation in frontoparietal and cingulo-opercular network regions would predict CBT outcomes.
(b) Altered structural connectivity in the corpus callosum and in tracts within frontoparietal and cingulo-opercular networks that are functionally altered in OCD.
(c) Alternative in structural connectivity would also predict CBT outcomes.
(d) Characterised effect size and sensitivity/specificity of associations between treatment outcomes and brain structure.
55 unmedicated 7- to 18-year-olds participated in this study, including 28 patients with OCD and 27 healthy participants. Participants were clinically assessed using the Anxiety and Related Disorders Interview Schedule (ADIS) while OCD symptom severity was assessed using the Children's Yale-Brown Obsessive-Compulsive Scale (CY-BOCS). Patients exhibiting no change or worsening of symptoms (CY-BOCS) after 6 weeks of treatment were offered the option of psychopharmacological intervention. CYBOCS scores were the primary outcome measure assessed at pre-, mid-, and post-treatment. CBT 'responders' were defined by a post-treatment CY-BOCS ≤ 12.
It was discovered that 9 cortical regions showed significant false-discovery rate (FDR)-corrected thickness 9-time interactions predicting CY-BOCS scores. These included the left parietal lobe (angular and supramarginal gyri [SMG]), right insular cortex, left middle and superior frontal, left precentral, left superior temporal, and left and right lingual gyri. For all nine regions, patients with the thinnest regional cortex showed the greatest symptom decline with treatment. Thickness in these nine regions jointly predicted a large portion of the variance in post-treatment CY-BOCS scores.
In a follow-up vertex-wise analysis, one left SMG cluster was significantly related to CY-BOCS improvement (difference scores). This cluster significantly predicted post-treatment CY-BOCS score such that 0.04mm of the thinness of cortex was associated with 1 point lower post-treatment CY-BOCS. It also predicted CBT response in logistic regression such that 0.01mm thinner cortex is associated with 1.19 times greater odds of a response. Comparing left SMG thickness between responders and non-responders to CBT indicated a large effect size. Additionally, in a ROC analysis, thresholding left SMG thickness at 2.77 mm was 72.22% specific and 90.00% sensitive in predicting response, which was significantly more discriminating than pretreatment CY-BOCS scores. Diffusion analysis predicted out of 10 connections, medial ACC-putamen showed a significant count 9-time interaction, such that fewer streamline counts predicted greater decline in symptoms overtreatment, but this did not pass FDR. Further, having fewer medial ACC-putamen streamlines predicted greater reductions in post-treatment CY-BOCS.
It was concluded that:
• While CBT is an effective, first-line treatment, not all pediatric patients with OCD respond. Neuroscience research may elucidate pretreatment markers to identify patients most likely to respond well.
• Cortical thickness in nine frontoparietal brain regions, particularly supramarginal gyrus, predicted response to CBT.
• Novel alterations in cingulo-opercular structural connectivity were also identified in patients with OCD compared with healthy children.
• Structural features of task control circuits may aid in identifying which pediatric patients respond best to CBT.
Source: Journal of child psychology and psychiatry. Pagliaccio D, Cha J, He X, Cyr M, Yanes-Lukin P, Goldberg P, Fontaine M, Rynn MA, Marsh R. Structural neural markers of response to cognitive behavioral therapy in pediatric obsessive-compulsive disorder. J Child Psychol Psychiatry. 2020 Dec;61(12):1299-1308. doi: 10.1111/jcpp.13191. Epub 2019 Dec 31. PMID: 31889307; PMCID: PMC7326644.
M.B.B.S, M.D. Psychiatry
M.B.B.S, M.D. Psychiatry (Teerthanker Mahavir University, U.P.) Currently working as Senior Resident in Department of Psychiatry, Institute of Human Behaviour and Allied Sciences (IHBAS) Dilshad Garden, New Delhi. Actively involved in various research activities of the department.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


