- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Key Scores Independently Predict 90-Day Mortality After Pancreaticoduodenectomy: Study
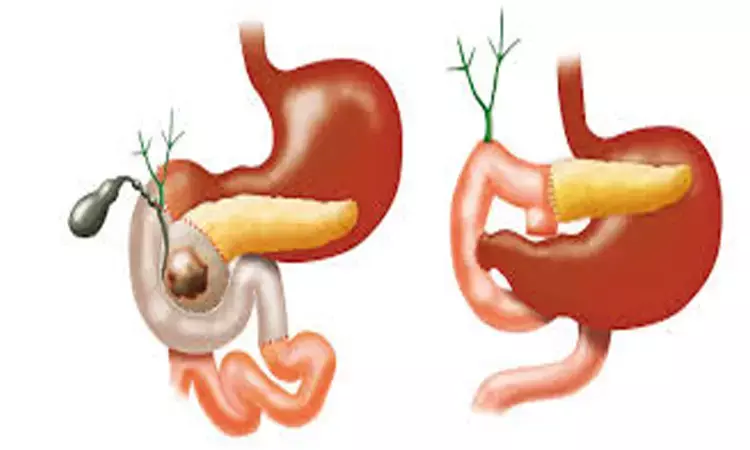
Pancreaticoduodenectomy (PD) in patients with periampullary cancer remains a procedure that holds a lot of risk of mortality in the immediate postoperative period; this study has found that some simple clinical variables can predict this mortality. It has been made clear that the risk of mortality in the 90 days post-PD is significantly increased by higher MELD-Na scores, higher Charlson Comorbidity Index after adjustment for age, and higher neutrophil/lymphocyte ratio. The study was published in BMC Surgery.
Periampullary malignancies commonly need PD as the only potentially curative therapy. However, the issue of postoperative mortality is of great concern. This retrospective study that covered more than a decade sought to find predictors of 90-day mortality in 105Patients who underwent a PD procedure between January 2010 and August 2022. From the conclusion that MELD-Na, ACCI, and NLR independently predict early postoperative deaths, it is clear that early on in the article, the importance of a compounded evaluation of the nature of the liver, the degree of comorbidities, and the levels of systemic inflammation is suggested.
This trial involved 105 patients who met the criteria for pancreaticoduodenectomy in relation to periampullary cancer. The patients could be categorized based on outcomes into group I, consisting of patients who had 90 days of operative mortality, totaling 17 individuals (16.2%), whereas group II consisted of patients who were discharged successfully beyond 90 days, totaling 88 patients (83.8%).
In addition to traditional clinical variables, three composite scores were incorporated into the analysis as follows: the Model for End-Stage Liver Disease-Sodium score (MELD-Na score), age-adjusted Charlson Comorbidity Index (ACCI), and the neutrophil-lymphocyte ratio (NLR). Survival analysis was conducted by means of the Kaplan-Meier method, and Cox proportional hazard analysis was applied for the identification of variables related to early postoperative deaths.
Results
• Univariable analysis showed age, sex, blood albumin concentrations, NLR, MELD-Na score, and ACCI were all highly associated with 90-day mortality after PD (p < 0.05).
• Nevertheless, multivariable analysis revealed three variables that had a particularly strong association with 90-day mortality.
• MELD-Na on admission had the highest hazard ratio (HR) at 10.75 (95%CI: 2.82-61.30, p = 0.001) for mortality.
• The ACCI variable also had a very high hazard ratio at 9.30 (95%CI: 2.30-46.05, p < 0.001).
• Systemic inflammation, indicated by the high NLR value, was an independent predictor, with a hazard ratio of 7.81 (95%CI: 1.98-48.38, p = 0.005).
• These results suggest that PB+ patients with poor liver function, high comorbidity indices, and high levels of inflammation are at much greater risk of early postoperative death after PD.
This confirms MELD-Na score, age-adjusted Charlson Comorbidity Index, and neutrophil-lymphocyte ratio to also be independent predictors of mortality at 90 days post-pancreaticoduodenectomy for periampullary cancer. Early preoperative risk assessment with these scoring systems and a multidisciplinary approach might also assist with lowering the mortality that occurs postoperatively.
Reference:
Yur, M., Aygen, E., İlhan, Y.S. et al. Risk factors for 90-day mortality after pancreaticoduodenectomy. BMC Surg (2025).https://doi.org/10.1186/s12893-025-03461-z
Dr Riya Dave has completed dentistry from Gujarat University in 2022. She is a dentist and accomplished medical and scientific writer known for her commitment to bridging the gap between clinical expertise and accessible healthcare information. She has been actively involved in writing blogs related to health and wellness.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


