- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Liposomal bupivacaine not superior to standard formulation for pain control after truncal incisions: JAMA
USA: Liposomal bupivacaine is not superior to standard bupivacaine formulation for postoperative pain control in major truncal surgery, finds a recent study in the journal JAMA Network Open.
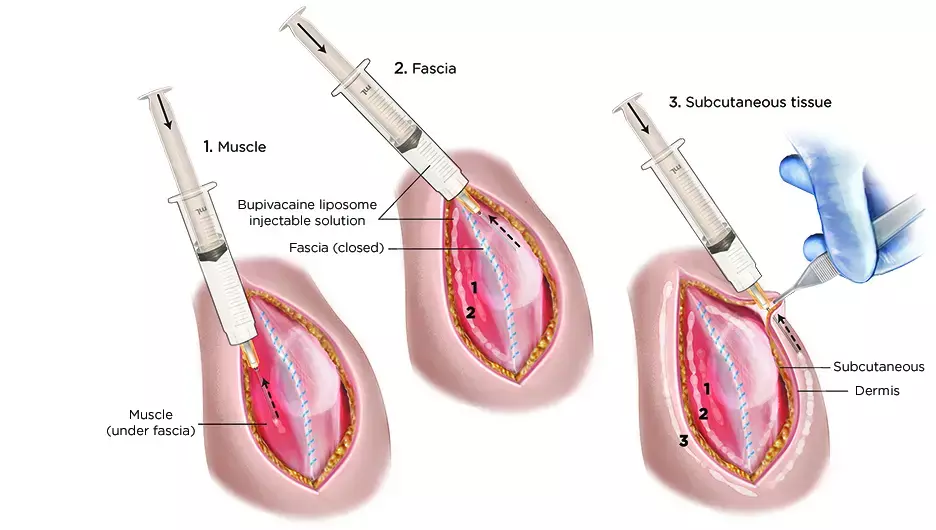
The pain relief effect of a more expensive formulation of bupivacaine, liposomal bupivacaine, is purported to last 3 days compared to standard bupivacaine whose effect lasts for 8 hours. However, its effectiveness is not known in truncal incisions for cardiothoracic or vascular operations.
Harleen K. Sandhu, McGovern Medical School at the University of Texas Health Science Center at Houston, and colleagues, therefore, aimed to compare the effectiveness of single-administration standard bupivacaine vs liposomal bupivacaine in patients undergoing truncal incisions.
For the purpose, the researchers performed a randomized clinical trial. It enrolled patients undergoing sternotomy, thoracotomy, minithoracotomy, and laparotomy from a single cardiovascular surgery department in an academic medical center center between November 2012 and June 2018.
The study was powered to detect a Cohen effect size of 0.35 with a power of greater than 80%.
280 patients were randomized to receive either single-administration standard bupivacaine (n=140) or liposomal bupivacaine (n=140).
Pain was assessed over 3 postoperative days by the Numeric Rating Scale (NRS). Adjunctive opioids were converted to morphine equivalents units (MEU). NRS scores were compared using Wilcoxon rank-sum (3-day area under the curve) and 2-way nonparametric mixed models (daily scale score) to assess time-by-group interaction.
Key findings of the study include:
- Irrespective of treatment assignment, pain decreased by a mean of approximately 1 point per day over 3 days (β = −0.87).
- Incision type was associated with pain with patients undergoing thoracotomy (including minithoracotomy) reporting highest median (interquartile range [IQR]) pain scores on postoperative days 1 (liposomal vs standard bupivacaine, 6 vs 5, Wilcoxon rank-sum) and 2 (liposomal vs standard bupivacaine, 5 vs 4, Wilcoxon rank-sum) but not day 3 (liposomal vs standard bupivacaine, 3 vs 3, Wilcoxon rank-sum), irrespective of treatment group.
- Median (IQR) 3-day cumulative NRS was 12.0 for bupivacaine and 13.5 for liposomal bupivacaine. Furthermore, use of opioids was greater following liposomal bupivacaine compared with standard bupivacaine (median [IQR], 41.5 MEU vs 33.0 MEU, Wilcoxon rank-sum).
- On multivariable analysis, no interaction by incision type was observed for mean pain scores or opioid use.
"In this randomized clinical trial involving truncal incisions for cardiovascular procedures, liposomal bupivacaine did not provide improved pain control and did not reduce adjunctive opioid use compared with conventional bupivacaine formulation over 3 postoperative days," wrote the authors.
The study titled, "Effectiveness of Standard Local Anesthetic Bupivacaine and Liposomal Bupivacaine for Postoperative Pain Control in Patients Undergoing Truncal Incisions: A Randomized Clinical Trial," is published in the journal JAMA Network Open.
DOI: https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2777506
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


