- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Tumor vessel invasion independent risk factor affecting prognosis of Gastric cancer: Study
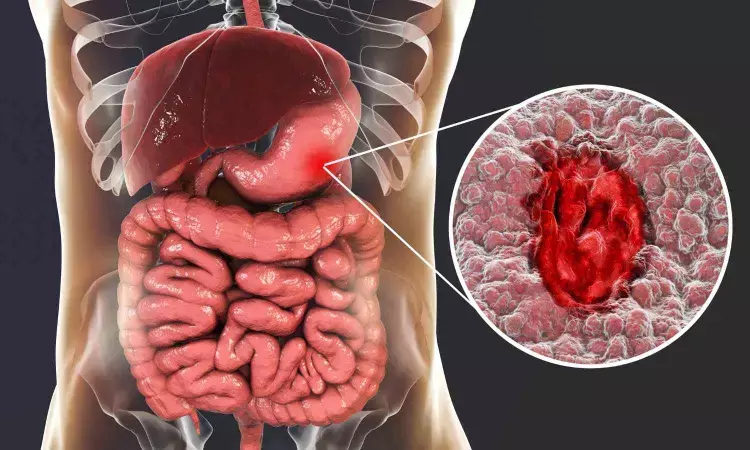
A new study published in the World Journal of Surgical Oncology found that vessel invasion (VI) is a risk factor that affects the outcome of gastric cancer (GC) and is linked to several pathological variables. The fifth most frequent malignant tumor in the world is gastric cancer that causes around 700,000 deaths and 1,000,000 new cases annually.
Tumors within the blood vessels or lymphatic system are referred to as vessel invasion (VI). As cancer progresses, tumor cells infiltrate the blood vessel and lymphatic vessel around the tumor, which is a critical route for tumor growth and dissemination. Tumor metastasis and recurrence are significantly influenced by VI formation. This study by Qiannan Wang and team investigated the possible role of VI and determined whether it may be used in conjunction with more conventional clinicopathological criteria to evaluate the prognosis of GC.
The retrospective analysis and filtering based on certain inclusion and exclusion criteria were done on 3600 instances of GC patients who had radical gastrectomy at the gastrointestinal surgery department of the First Affiliated Hospital of Naval Medical University between June 2014 and June 2019. The patients were divided into 2 groups based on whether or not VI was present, and a one-to-one propensity score matching (PSM) was used to create 724 patients in each group to reduce the possibility of selection bias related to VI.
Data from 3,205 GC patients were evaluated to look for variations in VI positivity across different clinicopathological factors. To examine the relationship between clinicopathological variables and prognosis, both univariate and multivariate Cox regression models were used. Plotting Kaplan-Meier survival curves helped to better illustrate the results.
This study comprised a total of 3205 individuals, of whom 2216 (69.1%) were VI-negative and 989 (30.9%) were VI-positive. Age, body mass index (BMI), tumor location, pTNM stage, perineural invasion (PI), Lauren classification, and tumor deposit (TD) were shown to be substantially correlated with the VI-positive group, but not with gender or basic illness.
Prior to and during PSM matching, VI-positive patients had a more severe survival rate than VI-negative patients. The patients with VI had a 5-year survival rate of 58.03%, whereas the individuals without VI had a higher rate of 66.25% after PSM.
Furthermore, VI was shown to be a separate risk factor for prognosis by multivariate analysis following matching. Overall, the presence of VI in GC patients is impacted by a variety of parameters, including age, depth of infiltration, BMI, number of lymph node metastases, PI, gastrectomy site, Lauren classification, and TD.
Source:
Wang, Q., Liu, Z., Han, J., Gao, Y., Shao, Y., Cai, H., & Yin, K. (2024). Vessel invasion is a risk factor for gastric cancer: a retrospective analysis study. In World Journal of Surgical Oncology (Vol. 22, Issue 1). Springer Science and Business Media LLC. https://doi.org/10.1186/s12957-024-03604-1
Neuroscience Masters graduate
Jacinthlyn Sylvia, a Neuroscience Master's graduate from Chennai has worked extensively in deciphering the neurobiology of cognition and motor control in aging. She also has spread-out exposure to Neurosurgery from her Bachelor’s. She is currently involved in active Neuro-Oncology research. She is an upcoming neuroscientist with a fiery passion for writing. Her news cover at Medical Dialogues feature recent discoveries and updates from the healthcare and biomedical research fields. She can be reached at editorial@medicaldialogues.in
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


