- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Drug-coated balloon angioplasty benefits dysfunctional dialysis fistulas patients: NEJM
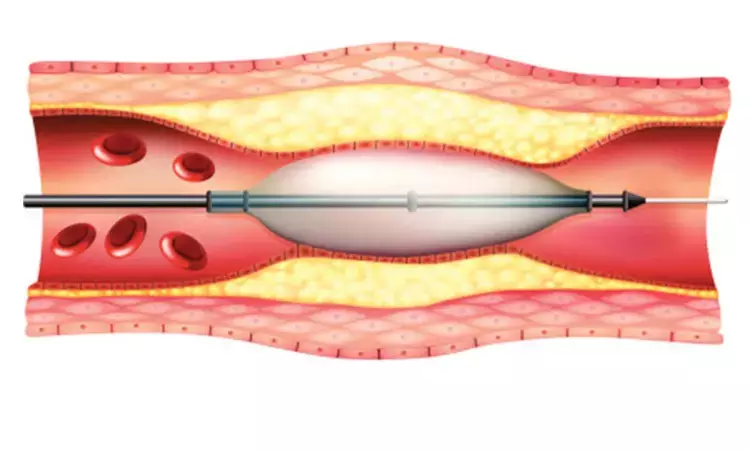
USA: Treatment with a drug-coated balloon is beneficial over standard angioplasty for the treatment of stenotic lesion in patients on hemodialysis who had a dysfunctional arteriovenous fistula, according to a recent study in NEJM.
The current recommended treatment for dysfunctional hemodialysis fistulas is standard percutaneous transluminal angioplasty but the long-term outcomes of this treatment are poor. Delivery of antirestenotic agent paclitaxel via drug-coated balloons may be associated with improved outcomes. Robert A. Lookstein, Icahn School of Medicine at Mount Sinai, and colleagues conducted a prospective, single-blinded, 1:1 randomized trial, and enrolled 330 participants at 29 international sites.
The study included patients with new or restenotic lesions in native upper-extremity arteriovenous fistulas. A total of 330 participants were randomly assigned to receive treatment with a drug-coated balloon (n=170) or a standard balloon (n=160) after successful high-pressure percutaneous transluminal angioplasty.
The primary effectiveness endpoint was target-lesion primary patency, defined as freedom from clinically driven target-lesion revascularization or access-circuit thrombosis during the 6 months after the index procedure. The primary safety endpoint, serious adverse events involving the arteriovenous access circuit within 30 days, was assessed in a noninferiority analysis (margin of noninferiority, 7.5 percentage points).
Key findings of the study include:
- During the 6 months after the index procedure, target-lesion primary patency was maintained more often in participants who had been treated with a drug-coated balloon than in those who had been treated with a standard balloon (82.2% [125 of 152] vs. 59.5% [88 of 148]; difference in risk, 22.8 percentage points).
- Drug-coated balloons were noninferior to standard balloons with respect to the primary safety endpoint (4.2% [7 of 166] and 4.4% [7 of 158], respectively; difference in risk, −0.2 percentage points).
- Sensitivity analyses confirmed the results of the primary analyses.
"Drug-coated balloon angioplasty was superior to standard angioplasty for the treatment of stenotic lesions in dysfunctional hemodialysis arteriovenous fistulas during the 6 months after the procedure and was noninferior with respect to access circuit–related serious adverse events within 30 days," concluded the authors.
The study, "Drug-Coated Balloons for Dysfunctional Dialysis Arteriovenous Fistulas," is published in the New England Journal of Medicine
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


