- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
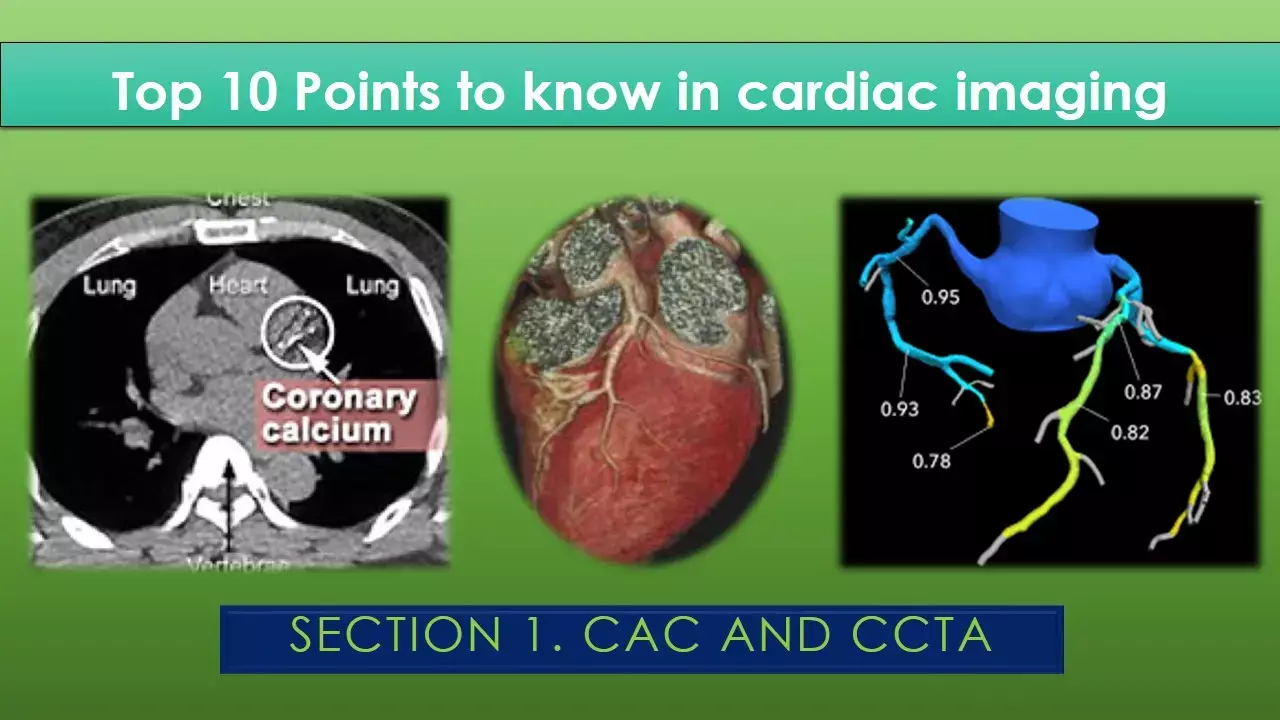
Top 10 messages from cardiac imaging: CAC and CCTA
Knowing the patient's current cardiovascular disease (CVD) status, as well as the patient's current and future CVD risk, helps the clinician make more informed patient-centered management recommendations towards the goal of preventing future CVD events. In this regard, American Society for Preventive Cardiology (ASPC) has released a state of the art review that summarizes the key points describing the utility and application of commonly used cardiac imaging investigations with respect to preventive and diagnostic cardiology.
The review has been written by Bays et al and was recently published in American Journal of Preventive Cardiology.
In this series of three sections, we will describe the most significant messages from these recommendations, beginning with this first section on coronary artery calcium assessment and coronary artery CT angiography. The next 2 sections will detail the key takeaways for echocardiography, nuclear imaging, cardiac MRI and cardiac catheterization.
This review is aimed to benefit cardiologists as well as practising physicians by providing a crisp nutshell of knowledge about contemporary diagnostic modalities.
1. Coronary calcium scoring:
A coronary artery calcium (CAC) score utilizes CT to assess the amount of calcium found in coronary arteries. Arterial calcium reflects vascular injury, inflammation, and repair. Coronary calcium is a marker of plaque burden. The earliest stage of positive remodelling is undetectable by any imaging modality including the gold standard invasive angiography.
This pathogenic clinical scenario is often clarified by CAC. Assessment of coronary artery calcium is most often performed by multidetector computed tomography (MDCT); CAC does not require contrast and radiation exposure is much less than coronary CT angiography (1mSv vs. up to 5mSv for the latter).
Top 10 key points about CAC are summarised in the table below.
1. For most patients, the higher the CAC score, the higher the atherosclerotic burden and the higher the risk of a subsequent CVD event. |
| 2. the MESA and ASTRO-CHARM risk calculators already use CAC as one of the parameters to calculate ASCVD risk score. |
| 3. Patients most likely to benefit from CAC testing include asymptomatic individuals not known to have CVD, but who are 40 years and older without diabetes mellitus, individuals in whom primary CVD prevention therapeutics are being considered (e.g., statins), and/or individuals having borderline to intermediate 10-year ASCVD risk estimate of 5 – 20%. |
| 4. CAC scoring is generally not recommended for patients at low, < 5% 10-year ASCVD risk or patients with known CVD or patients at high, greater than 20% 10-year ASCVD risk. |
| 5. In appropriate individuals, statin therapy is strongly indicated when the CAC score is > 100 AU, or ≥ 75th percentile |
| 6. A CAC score of zero AU suggests a low risk of subsequent CVD event (i.e., acute myocardial infarction, coronary death, stroke, revascularization) over at least the next 8 years. |
| 7. A CAC score of ≥ 1000 AU represent a unique very high-risk phenotype of extreme coronary atherosclerosis with mortality outcomes commensurate with high-risk secondary prevention patients. |
| 8. Given that CAC scores are unlikely to regress, CAC scores do not track response to cardiovascular preventive therapy (i.e., response to statins). |
| 9. Individuals with a negative CAC score of potential unclear clinical significance include younger individuals who may have non-calcified atherosclerosis, patients with microvascular dysfunction, such as some women (and men) with non-obstructive ischemic heart disease (as may be assessed by PET). |
| 10. A low CAC score should not negate CVD risk factor management if other strong risk factors or risk enhancers are present. |
2. Coronary computed tomography angiography (CCTA)
Atherosclerotic progression begins with early reversible subendothelial lipid accumulation, early inflammation, and minimal fibrosis. Further atherosclerotic progression may lead to lipid plaque, chronic inflammation, fibrosis, and perivascular adipose tissue remodeling – which if untreated, may ultimately become irreversible. CCTA can measure lipid rich plaque, as well as perivascular fat and inflammation.
When combined with FFR, CCTA can help determine the functional significance of stenotic lesions. With use of an iodine intravenous contrast agent, CCTA can visualize the coronary artery lumen. The key clinical aspects of this technique are summarised in the table below.
| 1. CCTA has a high negative predictive value, such that if negative, then clinically meaningful CVD risk. CCTA may be especially valuable in assessing patients with chest pain or related symptoms, but without known CHD and who are at low to intermediate CVD risk. CCTA guided changes in management can improve clinical outcomes. |
| 2. CCTA is a potential non-invasive imaging test of choice in patients with symptoms of chest pain where obstructive CAD cannot be reasonably established by history and physical exam alone |
| 3. CCT has high negative predictive value for left main disease. |
| 4. Evaluation of the severity of coronary stenosis can be derived from estimating pressure differences via "virtual" fractional flow reserve derived from CCTA (FFRCT). |
| 5. CCTA can assess non-obstructive coronary artery plaque, which can inform CVD preventive management. |
| 6. Poor image quality and severe calcification can overestimate CCTA coronary artery stenosis. |
| 7. CCTA is not recommended in patients with extensive coronary calcification, arrhythmias, significant obesity, and in patients unable to hold their breath – all which may adversely affect image quality. |
| 8. CCTA image quality may be impaired in patients with prior cardiac revascularization. |
| 9. The contrast with CCTA is contraindicated in patients with contrast dye allergies. |
| 10. Contrast (i.e., iodine) induced acute kidney injury occurs due to contrast-mediated hypoperfusion, direct tubular toxicity, and vasoconstriction. CCTA contrast should be used with caution in patients with kidney insufficiency and warrants adequate fluid intake in those receiving contrast. |
Cardiac imaging helps assess the degree of CVD, which is important in stratifying current CVD risk and determining management strategies toward preventing future CVD events. CVD risk factor management is often more aggressive and often prioritized to patients most likely to benefit, which often includes those with diagnosed CVD or otherwise at increased CVD risk.
Source: https://doi.org/10.1016/j.ajpc.2021.100176
MBBS, MD , DM Cardiology
Dr Abhimanyu Uppal completed his M. B. B. S and M. D. in internal medicine from the SMS Medical College in Jaipur. He got selected for D. M. Cardiology course in the prestigious G. B. Pant Institute, New Delhi in 2017. After completing his D. M. Degree he continues to work as Post DM senior resident in G. B. pant hospital. He is actively involved in various research activities of the department and has assisted and performed a multitude of cardiac procedures under the guidance of esteemed faculty of this Institute. He can be contacted at editorial@medicaldialogues.in.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


