- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Rivaroxaban helps in preventing LV thrombus formation in MI patients: JACC study
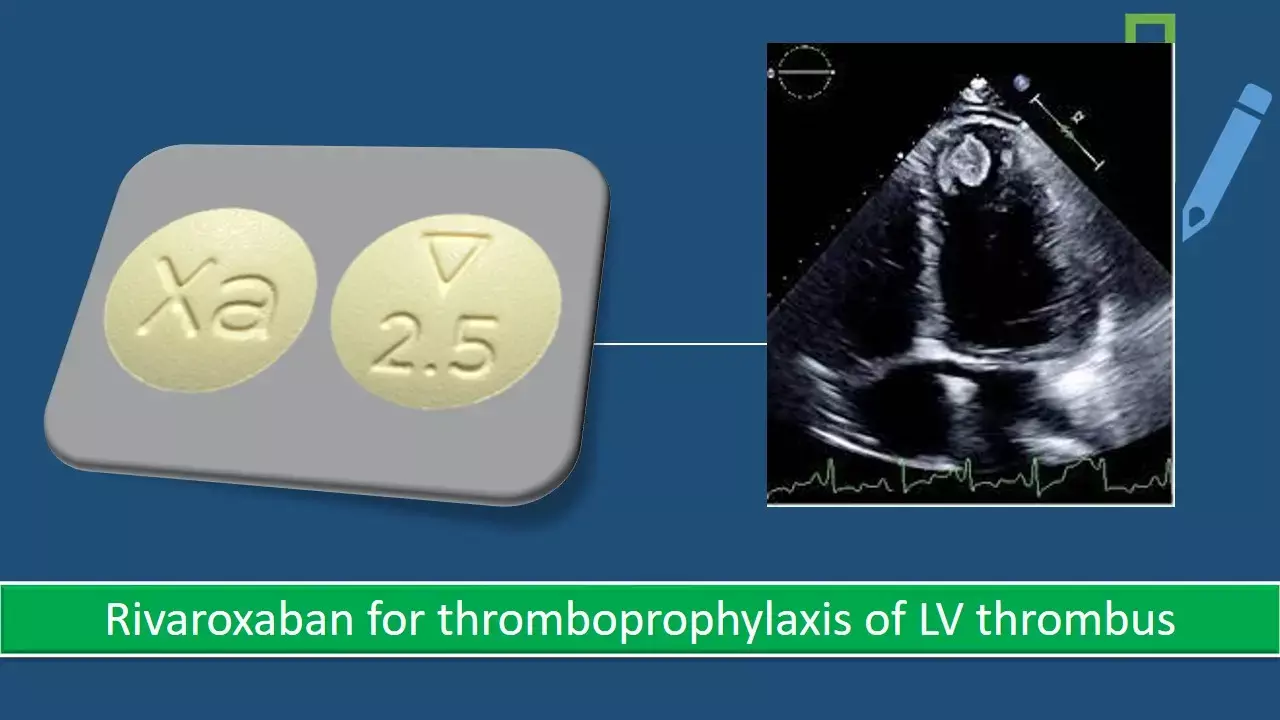
Left ventricular thrombus (LVT) usually appears within 1 month after ST-segment elevation myocardial infarction (STEMI) with an incidence still ranging between 4-26% in the current primary PCI era. LVT usually complicates acute myocardial infarction and is associated with a higher incidence of poor outcomes. While the use of VKA antagonists has not been successful prophylactic strategy in this regard, a recent research has shown a useful role of low dose rivaroxaban in addition to DAPT to prevent LVT formation.
In the latest issue of JACC Cardiovascular Interventions, Zhang et al have shown that short-duration addition of low-dose rivaroxaban to DAPT could reduce LVT formation by as much as 92% in patients with anterior STEMI following primary percutaneous coronary intervention when compared to those taking DAPT alone.
For left ventricle thromboprophylaxis in high risk patients with AWMI, clinicians continue to face uncertainty in decision making. However, the advent of direct oral anticoagulants (DOACs), which attenuate fibrin formation by selective inhibition of factor Xa or thrombin, has renewed the interest in inhibition strategies that combine DAPT with an anticoagulant drug in this area.
The authors randomly assigned 279 patients with anterior STEMI who had undergone primary PCI to receive, in a 1:1 ratio, low-dose rivaroxaban (2.5 mg twice daily for 30 days) and DAPT or only DAPT.
The primary efficacy outcome was the LVT formation within 30 days. Net clinical adverse events were assessed at 30 days and 180 days, including all-cause mortality, LVT, systemic embolism, rehospitalization for cardiovascular events, and bleeding.
The addition of low-dose rivaroxaban to DAPT reduced LVT formation within 30 days compared with only DAPT (0.7% vs 8.6). Net clinical adverse events were lower within 30 days in the rivaroxaban group versus those in the only DAPT group and remained relatively low throughout the follow-up period.
There were no significant differences in bleeding events between the 2 groups in 30 days and 180 days.
Due to poor outcomes after left ventricular thrombosis, estimating the risk of thrombus formation and embolization as well as the utility of prophylactic treatment remains critical. The net clinical benefit was measured by the composite of NACEs in this trial. The composite, which included all-cause mortality, LVT, SE, rehospitalization for cardiovascular events, and bleeding, favored the addition of rivaroxaban to DAPT in patients with anterior STEMI in the short duration.
Further studies are required to elucidate the mechanisms by which rivaroxaban favorably influences LVT formation in patients with anterior STEMI who had undergone interventional treatments. The duration of anticoagulation also needs to be further determined. But nonetheless, this study has shown a way forward for one of the most perplexing clinical situations i.e. how to provide thromboprophylaxis for LVT.
Source: JACC Cardiovascular Interventions: DOI: 10.1016/j.jcin.2022.01.285
MBBS, MD , DM Cardiology
Dr Abhimanyu Uppal completed his M. B. B. S and M. D. in internal medicine from the SMS Medical College in Jaipur. He got selected for D. M. Cardiology course in the prestigious G. B. Pant Institute, New Delhi in 2017. After completing his D. M. Degree he continues to work as Post DM senior resident in G. B. pant hospital. He is actively involved in various research activities of the department and has assisted and performed a multitude of cardiac procedures under the guidance of esteemed faculty of this Institute. He can be contacted at editorial@medicaldialogues.in.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


