- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Role of drug-induced sleep endoscopy in evaluation of positional vs non-positional OSA
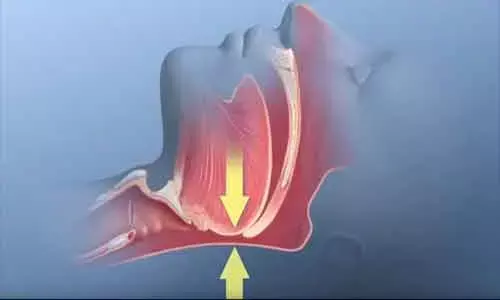
According to recent findings, it has been noted that a higher prevalence of velum concentric collapse, oropharyngeal lateral wall collapse, and tongue base anteroposterior collapse were observed in patients with non-positional OSA and oropharyngeal lateral wall collapse was the only anatomical predictor for non-positional dependency in OSA patients, as published in the Journal of Otolaryngology - Head & Neck Surgery.
Treatment modalities of OSAS are mainly composed of continuous positive airway pressure (CPAP), mandibular advancement devices (MAD), and upper airway surgery. CPAP is typically recommended as gold standard therapy for OSA. However, the mechanisms underlying positional and non-positional OSA are poorly understood, which might be attributable to distinct clinical characteristics and upper airway anatomy.
Hence, Ming-Chin Lan and colleagues from the Department of Otolaryngology-Head & Neck Surgery, Taipei Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, New Taipei City, Taiwan conducted the study to evaluate the anatomical differences between positional and non-positional OSA, and to identify the potential predictors for distinguishing between these two types of OSA.
A cross-sectional study of 230 consecutive patients with OSA undergoing DISE (Drug-induced Sleep Endoscopy) was carried out at a tertiary academic medical center. The factors correlating with positional and non-positional OSA were analyzed, including clinical characteristics, polysomnography data, and DISE findings.
The following results were observed-
a. Non-positional dependency was correlated with a higher BMI (p < 0.001), neck circumference (p < 0.001), modified Mallampati score (p = 0.003), AHI (p < 0.001), degree of velum concentric collapse (p = 0.004), degree of oropharyngeal lateral wall collapse (p < 0.001), and degree of tongue base anteroposterior collapse (p = 0.004).
b. Multivariate analysis revealed that oropharyngeal lateral wall collapse (OR = 1.90, p = 0.027) was the only anatomical factor significantly predicted non-positional dependency in OSA patients.
c. AHI (OR = 1.04, p < 0.001), although significant, made only a marginal contribution to the prediction of non-positional dependency.
Therefore, it was concluded that "oropharyngeal lateral wall collapse was identified as the only anatomical predictor for non-positional dependency in OSA patients. Therefore, further treatment modalities should address the distinct anatomical trait between positional and non-positional OSA."
Dr. Nandita Mohan is a practicing pediatric dentist with more than 5 years of clinical work experience. Along with this, she is equally interested in keeping herself up to date about the latest developments in the field of medicine and dentistry which is the driving force for her to be in association with Medical Dialogues. She also has her name attached with many publications; both national and international. She has pursued her BDS from Rajiv Gandhi University of Health Sciences, Bangalore and later went to enter her dream specialty (MDS) in the Department of Pedodontics and Preventive Dentistry from Pt. B.D. Sharma University of Health Sciences. Through all the years of experience, her core interest in learning something new has never stopped. She can be contacted at editorial@medicaldialogues.in. Contact no. 011-43720751
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


