- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Diagnosis and treatment of acute calculus cholecystitis: WSES 2020 Guideline
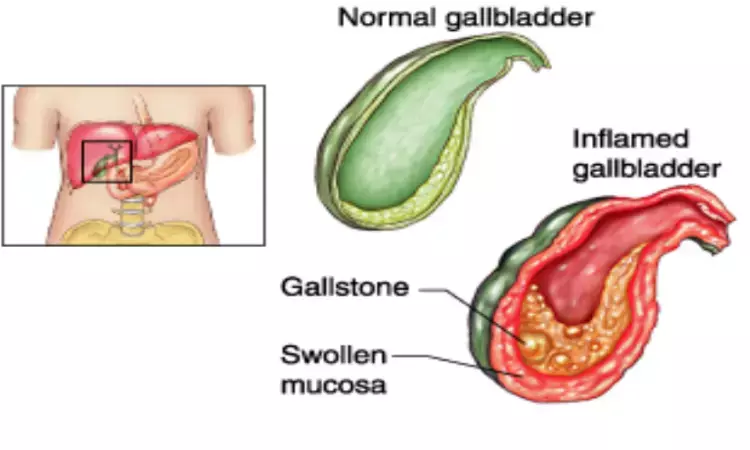
Italy: The World Society of Emergency Surgery (WSES) has released an updated guideline on the diagnosis and management of acute calculus cholecystitis (ACC)
Key recommendations include
Diagnosis of ACC
- As no feature has sufficient diagnostic power to establish or exclude the diagnosis of ACC, it is recommended not to rely on a single clinical or laboratory finding.
- For the diagnosis of ACC, we suggest using a combination of detailed history, complete clinical examination, laboratory tests and imaging investigations. However, the best combination is not known.
- The researchers recommend the use of abdominal ultrasound (US) as the preferred initial imaging technique, in view of its cost-effectiveness, wide availability, reduced invasiveness and good accuracy for gallstones disease.
- The use of further imaging is recommended for the diagnosis of ACC in selected patients, depending on local expertise and availability. Hepatobiliary iminodiacetic acid (HIDA) scan has the highest sensitivity and specificity for the diagnosis of ACC as compared to other imaging modalities. Diagnostic accuracy of computed tomography (CT) is poor. Magnetic resonance imaging (MRI) is as accurate as abdominal US.
Tools to Use for Suspicion and Diagnosis at Presentation
- The use of elevated LFTs or bilirubin is not recommended as the only method to identify CBDS (common bile duct stone) in patients with ACC, in which case we recommend performing further diagnostic tests.
- Consider the visualization of a stone in the common bile duct at transabdominal US as a predictor of CBDS in patients with ACC.
- An increased diameter of common bile duct, an indirect sign of stone presence, is not sufficient to identify ACC patients with CBDS and we therefore recommend performing further diagnostic tests.
- In order to assess the risk for CBDS, we suggest performing liver function tests (LFTs), including ALT, AST, bilirubin, ALP, GGT and abdominal US in all patients with ACC.
- Stratifying the risk of CBDS is suggested according to the proposed classification modified from the American Society of Gastrointestinal Endoscopy and the Society of American Gastrointestinal Endoscopic Surgeon Guidelines.
- The patients with moderate risk for CBDS are recommended to undergo one of the following: preoperative magnetic resonance cholangiopancreatography (MRCP), preoperative endoscopic ultrasound (EUS), intraoperative cholangiography (IOC), or laparoscopic ultrasound (LUS), depending on local expertise and availability.
- Patients with high-risk for CBDS are recommended to undergo preoperative ERCP, IOC or LUS, depending on the local expertise and the availability of the technique.
- Removing CBDS is recommended, either preoperatively, intraoperatively, or postoperatively, according to the local expertise and the availability of several techniques.
Source : World Journal of Emergency Surgery
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751
Next Story


