- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Mandibular advancement device improves daytime sleepiness in sleep apnea
Mandibular advancement devices (MADs) represent the main non-continuous positive airway pressure (non-CPAP) therapy for patients with obstructive sleep apnoea (OSA).
With the help of a mandibular advancement device (MAD), daytime sleepiness of patients with obstructive sleep apnoea can be relieved.
Treatment with an MAD is not inferior to positive airway pressure (PAP) therapy with a sleep mask. This is the conclusion reached by the German Institute for Quality and Efficiency in Health Care (IQWiG) in its final report on the benefit of MAD.
Breathing pauses disturb sleep and lead to daytime sleepiness
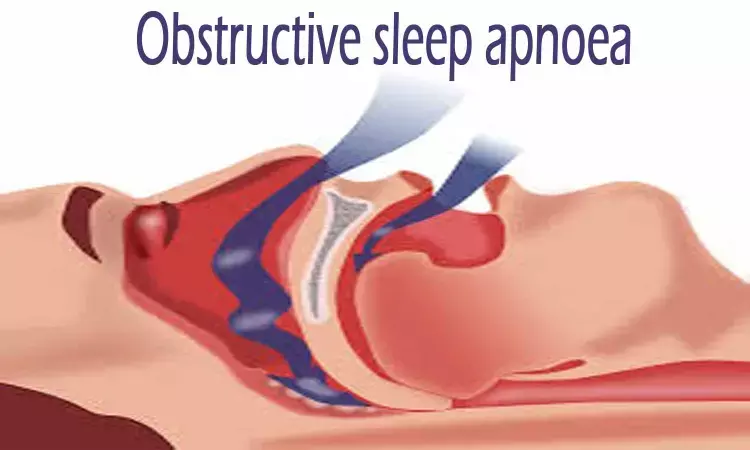
Obstructive sleep apnoea is characterized by a recurrent obstruction (= narrowing / blockage) of the upper airway during sleep. It occurs when the upper airway muscles become flaccid. This narrows the airway in the pharynx or even blocks it completely, resulting in loud snoring sounds when breathing in and out. People with obstructive sleep apnoea - usually without noticing it - have difficulties breathing while sleeping, including breathing pauses, and are very sleepy during the day. In the long term, this increases the risk of other diseases and can have a huge impact on quality of life. It is estimated that about 5% of men and 3% of women suffer from obstructive sleep apnoea.
A mandibular advancement device keeps the airways open mechanically
The treatment of obstructive sleep apnoea depends on the severity of the disease. If it is mild, conservative measures such as weight reduction, sleep hygiene measures (no alcohol, no smoking) or positional therapy (avoiding lying on the back while sleeping) can alleviate the symptoms. For a higher degree of severity, PAP therapy with a sleep mask is used as standard treatment, where ventilation with positive pressure is used to keep the patients' airways open.
According to the relevant clinical practice guideline, mild to moderate obstructive sleep apnoea can also be treated with an MAD. The plastic splint in the mouth, fitted by a dentist or orthodontist, then ensures that the lower jaw is held further forward, keeping the upper airway mechanically open. This method is usually well tolerated and is in many cases preferred by patients over PAP therapy. However, MAD treatment is not suitable for all patients: In cases of toothlessness, insufficient remaining teeth or pronounced periodontitis, for example, the plastic splint cannot be worn.
Treatment with an MAD is not inferior to PAP therapy
On behalf of the Federal Joint Committee (G-BA), IQWiG investigated in 2 research questions whether wearing an MAD is beneficial for obstructive sleep apnoea:
In comparison to no treatment or treatment with a placebo splint (research question 1), IQWiG researchers infer an indication of a benefit of wearing an MAD for the patient-relevant outcome "daytime sleepiness". This benefit is not challenged by the results on other patient-relevant outcomes (including sleep quality, cognitive performance, depressive symptoms and headaches). No data were available for the outcomes of overall mortality or survival and cardiovascular morbidity. In comparison with PAP therapy (research question 2), the IQWiG researchers infer an indication of non-inferiority of MAD versus PAP therapy for the patient-relevant outcome "daytime sleepiness". With regard to other patient-relevant outcomes, there was no disadvantage of MAD compared with PAP therapy either. No usable data were available for the outcomes of overall mortality or survival and cardiovascular morbidity.
The conclusions on the benefit of MAD are based on the results of 18 randomized controlled trials (RCTs) included in the assessment. To investigate the non-inferiority of MAD, the IQWiG project team was able to use the results from 17 RCTs. Many of the studies did not differentiate according to the severity of obstructive sleep apnoea, but included all persons with obstructive sleep apnoea or summarized several degrees of severity. This includes persons with mild to moderate obstructive sleep apnoea, who, according to the G-BA's commission, should be the focus of the benefit assessment.
After the hearing: "hint" becomes "indication"
In comparison with the preliminary report, the IQWiG project team upgraded the conclusions on the benefit of MAD from "hint" to "indication", both in comparison with no treatment or placebo (research question 1) and for the non-inferiority of MAD versus PAP therapy (research question 2). This also happened because, in the context of the hearing on the preliminary report, the participants submitting comments pointed out calculation errors in the probability calculations, which IQWiG has now corrected. Among other things, this resulted in different correlation coefficients for the assessments. In addition, a new study also provided additional evidence for research question 2 (MAD vs. PAP therapy). This led to more robust assessment results for both research questions regarding the outcome "daytime sleepiness".
for further references log on to:
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


