- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Balloon Angioplasty Plus Aggressive Medical Management Reduces Stroke Risk in Intracranial Artery Stenosis: BASIS Trial
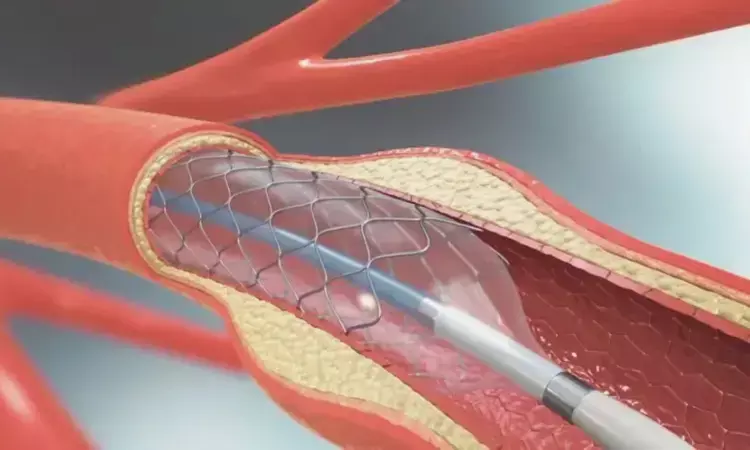
China: A recent study has provided new insights into treating symptomatic intracranial atherosclerotic stenosis (sICAS), revealing that balloon angioplasty combined with aggressive medical management significantly improves patient outcomes compared to medical management alone. The findings were from the BASIS (Balloon Angioplasty and Stenting for Intracranial Atherosclerosis) randomized clinical trial, which offers promising evidence for enhancing treatment strategies for this challenging condition.
"The findings indicate that combining balloon angioplasty with aggressive medical management could be an effective treatment for sICAS. However, stroke or death risk within 30 days following balloon angioplasty should be carefully considered in clinical practice," the researchers wrote in JAMA.
Intracranial artery stenosis is a condition where the arteries within the brain become narrowed, increasing the risk of stroke. Historically, medical management—often involving antiplatelet therapy and medications to control risk factors—has been the standard approach.
Previous randomized clinical trials have not shown that endovascular stenting is superior to aggressive medical management for patients with symptomatic intracranial atherosclerotic stenosis. However, balloon angioplasty has not been evaluated in a randomized clinical trial. Therefore, Xuan Sun, China National Clinical Research Center for Neurological Diseases, Beijing, China, and colleagues aimed to evaluate if combining balloon angioplasty with aggressive medical management offers superior outcomes compared to aggressive medical management alone for patients with sICAS.
For this purpose, the researchers conducted a randomized, open-label, blinded end-point clinical trial across 31 centers in China. The study recruited eligible patients aged 35 to 80 years with sICAS, defined as a recent transient ischemic attack (within 90 days) or ischemic stroke (14-90 days before enrollment), attributed to 70% to 99% atherosclerotic stenosis of a major intracranial artery. Patients had to be receiving treatment with at least one antithrombotic drug and/or standard risk factor management. Recruitment occurred between November 8, 2018, and April 2, 2022, with a final follow-up on April 3, 2023.
Participants were randomly assigned to either submaximal balloon angioplasty combined with aggressive medical management (n = 249) or aggressive medical management alone (n = 252). Aggressive medical management involved dual antiplatelet therapy for the initial 90 days and control of risk factors.
The primary outcome measures included a composite of any stroke or death within 30 days of enrollment or after balloon angioplasty of the qualifying lesion, as well as any ischemic stroke in the qualifying artery territory or revascularization of the qualifying artery from 30 days to 12 months after enrollment.
The study revealed the following findings:
- Among 512 randomized patients, 501 were confirmed eligible (mean age, 58.0 years; 31.5% were women) and completed the trial.
- The incidence of the primary outcome was lower in the balloon angioplasty group than in the medical management group (4.4% versus 13.5%; hazard ratio, 0.32).
- The respective rates of any stroke or all-cause death within 30 days were 3.2% and 1.6%.
- Beyond 30 days through 1 year after enrollment, the rates of any ischemic stroke in the qualifying artery territory were 0.4% and 7.5%, respectively, and revascularization of the qualifying artery occurred in 1.2% and 8.3%, respectively.
- The rate of symptomatic intracranial hemorrhage in the balloon angioplasty and medical management groups was 1.2% and 0.4%, respectively.
- In the balloon angioplasty group, procedural complications occurred in 17.4% of patients, and arterial dissection occurred in 14.5% of patients.
"In patients with sICAS, combining balloon angioplasty with aggressive medical management significantly reduced the risk of a composite outcome—including any stroke or death within 30 days, or an ischemic stroke or revascularization of the qualifying artery from 30 days to 12 months—compared to aggressive medical management alone," the researchers concluded.
Reference:
Sun X, Deng Y, Zhang Y, et al. Balloon Angioplasty vs Medical Management for Intracranial Artery Stenosis: The BASIS Randomized Clinical Trial. JAMA. Published online September 05, 2024. doi:10.1001/jama.2024.12829
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


