- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Endovascular Nimodipine Safe and Effective in Refractory post Aneurysmal Vasospasm
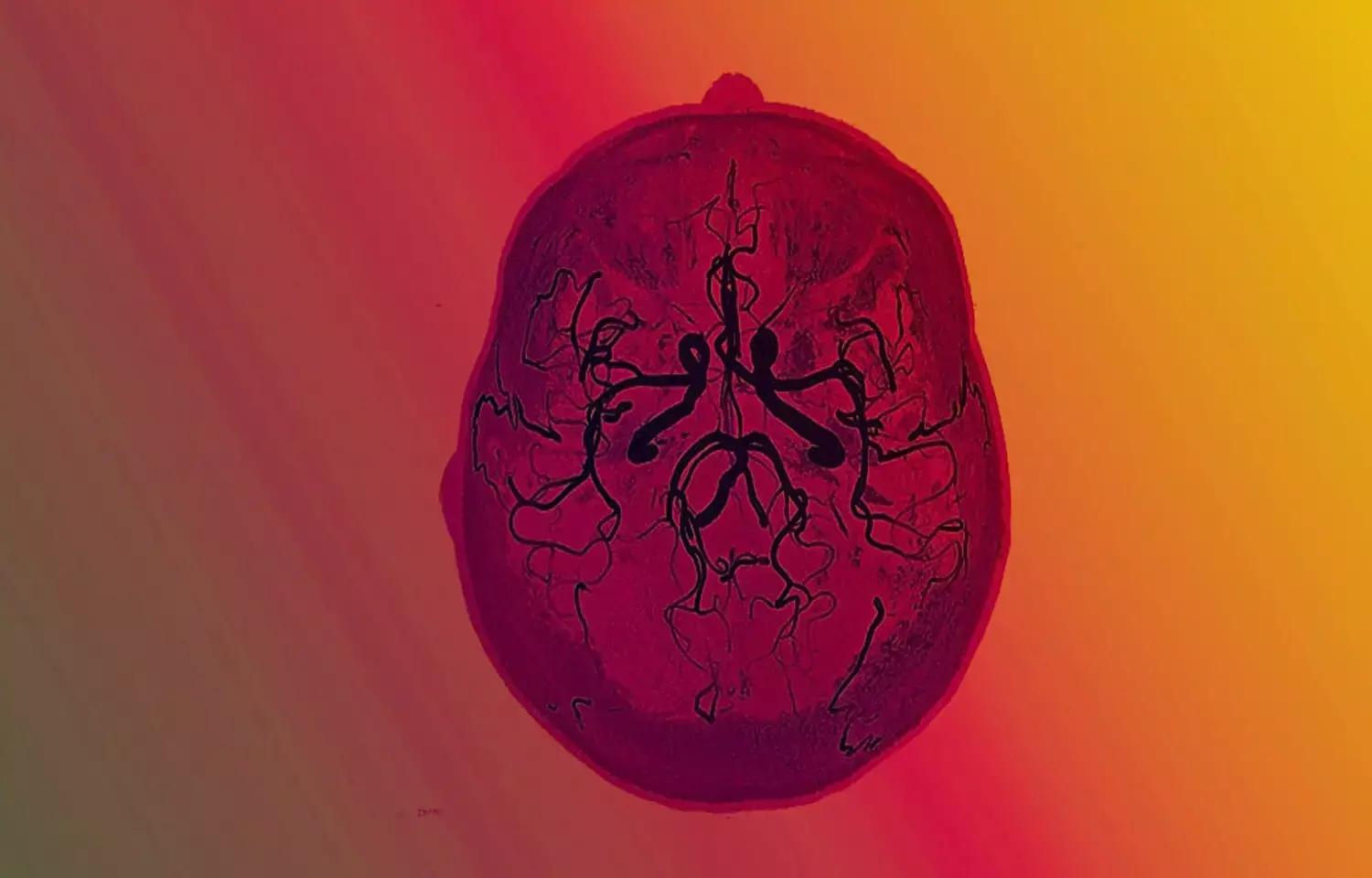
Endovascular chemical angioplasty using a Calcium channel blocker agent (Nimodipine) is a safe and efficient method for the treatment of refractory post aneurysmal SAH vasospasm, suggests a new study published in the Egyptian Journal of Neurosurgery.
Aneurysmal subarachnoid hemorrhage (SAH) is a catastrophic health burden with a high fatality rate and permanent disability complications. The incidence of SAH is 9/ 100,000 persons/year with regional variation with a 30 days fatality rate of 42%. It is an overwhelming problem with an overall prognosis depending on the volume of the initial bleeding, re-bleeding, vasospasm, the degree of delayed cerebral ischemia (DCI), hydrocephalus, and electrolyte disturbance. The extracranial complications may include myocardial ischemia with arrhythmias and neurogenic pulmonary edema.
Vasospasm is a major complication with increased rates of permanent disability and mortality following SAH. A deeper understanding of the pathophysiology and pathogenesis of the cerebral vasospasm is mandatory in dealing with DCI and making it one of the main targets of therapeutic goals. Oral and intravenous vasodilators are not always sufficient for most cases. For this reason, endovascular treatment of refractory cerebral vasospasm has become part of the standard treatment protocol in many neurosurgical centers. The most frequently used techniques aim to achieve arterial vessel dilatation using endovascular super selective intra-arterial administration of pharmacological agents, mechanical balloon angioplasty, or a combination of both. Endovascular balloon angioplasty techniques can be applied to only proximal vessel segments.
Sultan et al studied the angiographic and clinical effect of endovascular Intra-arterial injection of Nimodipine (IAN) on cerebral vasospasm after aneurysmal SAH that was resistant to systemic therapy. In their study 15 (50%) patients had a stable improvement in their clinical condition during the 24 h following vasospasm treatment with intra-arterial nimodipine. Twelve cases didn’t show any clinical improvement following the intra-arterial injection of nimodipine and 3 cases died during the following week. The mortality was related to the bad initial presentation and the refractory vasospasm.
The dose of the nimodipine was adjusted to work on reversing the angiographical vasospasm, to the same extent to avoid the hypotensive complication of the drug. In general, all patients received dosing ranging from 5- 8 mg as a total dose (1 to 2 mg loading as an initial dose and 4 mg/h as a maintenance dose provided no hypotension is monitored). There was no complication during all procedures other than hypotension which was rapidly corrected by intravenous fluids and vasoactive materials. The effect of IAN was monitored clinically, and the improved cases didn’t need another endovascular treatment session which reflects the durable effect of IAN.
Hypotension is well known as the most dominant side effect of systemically applied nimodipine. In their study population, 5 patients experienced an arterial blood pressure decrease of 20 mm Hg systolic after the initial bolus, despite the already-instituted hypertensive and hypervolemic therapy. In all patients, this effect was temporary and could easily be treated within minutes by adjusting the vasoactive medication. Nevertheless, this demonstrated that patients always need to be monitored during and after the IAN procedure.
In conclusion, IAN has a direct positive response in most patients with refractory vasospasm after standard therapy, improving both angiographic and clinical vasospasm. Although the data has some limits regarding the absence of PCT to assess the cerebral perfusion after the first 24 h yet results of the analysis suggest that intra-arterial nimodipine is effective and safe in selected cases of vasospasm following aneurysmal SAH. The search for better alternative dosing and ca channel blockers treatment strategies to reduce cerebral vasospasm and improve patients’ outcomes must be continued.
Reference
Sultan, A., Gaber, K. & Metwaly, T.I. Role of endovascular super selective intra-arterial injection of CA channel blocker agent (nimodipine) in management of cerebral vasospasm following aneurysmal SAH: a single institution experience. Egypt J Neurosurg 38, 9 (2023). Doi: https://doi.org/10.1186/s41984-023-00191-3
MBBS, DrNB Neurosurgery
Krishna Shah, MBBS, DrNB Neurosurgery. She did her MBBS from GMC, Jamnagar, and there after did direct 6 Year DrNB Neurosurgery from Sir Ganga Ram Hospital, Delhi. Her interests lie in Brain and Spine surgery, Neurological disorders, minimally invasive surgeries, Endoscopic brain and spine procedures, as well as research.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


