- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Severe glaucoma and younger age associated with microcystic macular edema: Study
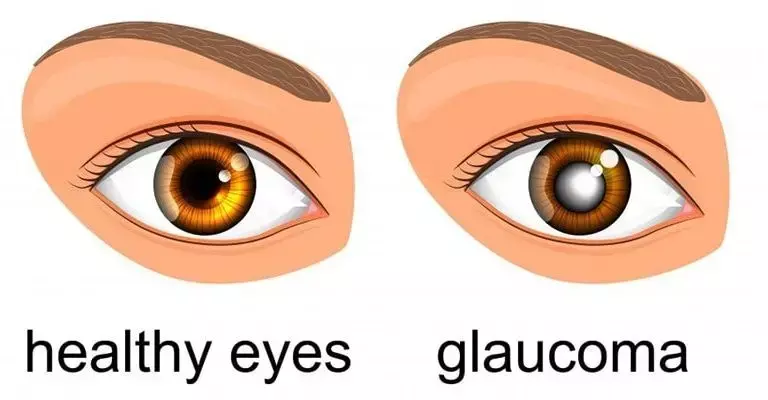
More severe glaucoma and younger age is associated with microcystic macular edema (MME) according to a recent study published in the British Journal of Opthalmology.
A study was conducted to identify clinical characteristics and factors associated with microcystic macular edema (MME) in patients with primary open-angle glaucoma (POAG).
They included 315 primary open-angle glaucomas (POAG) eyes between 2010 and 2019 with good-quality macular volume scans that had reliable visual fields (VF) available within 6 months in this observational retrospective cohort study. Eyes with retinal pathologies except for epiretinal membrane (ERM) were excluded. The inner nuclear layer was qualitatively assessed for the presence of microcystic macular edema (MME). Global mean deviation (MD) and Visual Field Index (VFI) decay rates, superior and inferior MD rates and pointwise total deviation rates of change were estimated with linear regression. Logistic regression was performed to identify baseline factors associated with the presence of MME and to determine whether microcystic macular edema (MME) is associated with progressive VF loss.
Results of the study are:
- 25 out of 315 eyes (7.9%) demonstrated microcystic macular edema (MME).
- The average (±SD) age and mean deviation (MD) in eyes with and without MME was 57.2 (±8.7) versus 62.0 (±9.9) years (p=0.02) and −9.8 (±5.7) versus −4.9 (±5.3) dB (p<0.001), respectively.
- Worse global MD at baseline (p=0.001) and younger age (p=0.02) were associated with the presence of microcystic macular edema (MME).
- ERM was not associated with the presence of MME (p=0.84) in this cohort.
- Microcystic macular edema (MME) was not associated with mean deviation (MD) and Visual Field Index (VFI) decay rates (p>0.49).
Thus, more severe glaucoma and younger age were associated with microcystic macular edema (MME). Microcystic macular edema (MME) was not associated with faster global Visual Field VF decay in this cohort. Microcystic macular edema (MME) may confound monitoring of glaucoma with full macular thickness.
Reference:
Risk factors for microcystic macular oedema in glaucoma by Golnoush Mahmoudinezhad et al. published in the British Journal of Ophthalmology.
doi: 10.1136/bjophthalmol-2021-320137
Keywords:
Golnoush Mahmoudinezha, Diana Salazar, Esteban Morales, Peter Tran, Janet Lee, Jean-Pierre primary open-angle glaucoma (POAG), Microcystic macular edema, MME, retinal pathologies, Visual Field, Visual Field index, decay rates, Hubschman, Kouros Nouri-Mahdavi, Joseph Caprioli, glaucoma, edema, Risk factors, macular, microcystic, British Journal of Ophthalmology
Dr. Shravani Dali has completed her BDS from Pravara institute of medical sciences, loni. Following which she extensively worked in the healthcare sector for 2+ years. She has been actively involved in writing blogs in field of health and wellness. Currently she is pursuing her Masters of public health-health administration from Tata institute of social sciences. She can be contacted at editorial@medicaldialogues.in.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


