- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
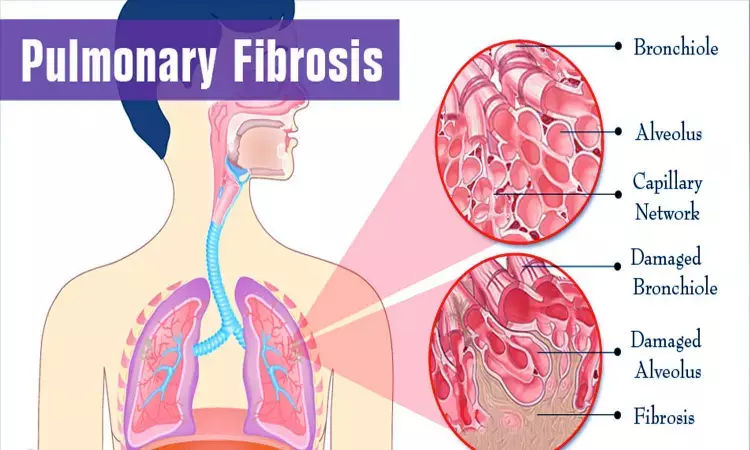
Antimicrobial therapy of not much benefit in idiopathic pulmonary fibrosis: JAMA
USA: The addition of co-trimoxazole (trimethoprim-sulfamethoxazole) or doxycycline did not significantly improve time to nonrespiratory hospitalization or death than usual care in adults with idiopathic pulmonary fibrosis, finds a recent study.
The findings, published in the journal JAMA, do not support treatment with these antibiotics for the underlying disease.
In patients with idiopathic pulmonary fibrosis, alteration in lung microbes is associated with disease progression. Fernando J. Martinez, New York Presbyterian Hospital/Weill Cornell Medicine, New York, and colleagues aimed to assess the effect of antimicrobial therapy on clinical outcomes.
For this purpose, the researchers conducted a pragmatic, randomized, unblinded clinical trial across 35 US sites. A total of 513 patients older than 40 years were randomized in the ratio of 1:1 to receive antimicrobials (n = 254) or usual care alone (n = 259) from August 2017 to June 2019.
Antimicrobials included co-trimoxazole (trimethoprim 160 mg/sulfamethoxazole 800 mg twice daily plus folic acid 5 mg daily, n = 128) or doxycycline (100 mg once daily if bodyweight <50 kg or 100 mg twice daily if ≥50 kg, n = 126). No placebo was administered in the usual care alone group.
The primary endpoint was time to first nonelective respiratory hospitalization or all-cause mortality.
The study was terminated for futility on December 18, 2019.
Key findings of the study include:
- After a mean follow-up time of 13.1 months (median, 12.7 months), a total of 108 primary end point events occurred: 52 events (20.4 events per 100 patient-years) in the usual care plus antimicrobial therapy group and 56 events (18.4 events per 100 patient-years) in the usual care group, with no significant difference between groups (adjusted HR, 1.04].
- There was no statistically significant interaction between the effect of the prespecified antimicrobial agent (co-trimoxazole vs doxycycline) on the primary end point (adjusted HR, 1.15 in the co-trimoxazole group vs 0.82 in the doxycycline group).
- Serious adverse events occurring at 5% or greater among those treated with usual care plus antimicrobials vs usual care alone included respiratory events (16.5% vs 10.0%) and infections (2.8% vs 6.6%); adverse events of special interest included diarrhea (10.2% vs 3.1%) and rash (6.7% vs 0%).
"Among adults with idiopathic pulmonary fibrosis, the addition of co-trimoxazole or doxycycline to usual care, compared with usual care alone, did not significantly improve time to nonelective respiratory hospitalization or death," wrote the authors. "These findings do not support treatment with these antibiotics for the underlying disease."
Reference:
The study titled, "Effect of Antimicrobial Therapy on Respiratory Hospitalization or Death in Adults With Idiopathic Pulmonary Fibrosis: The CleanUP-IPF Randomized Clinical Trial," is published in JAMA.
DOI: https://jamanetwork.com/journals/jama/fullarticle/2779827
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


