- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Tackling branch pulmonary artery atresia without open surgery, a case report
JACC case reports. A case report by Christopher J. Petit et al describes the use of direct percutaneous access to recanalize an atretic right pulmonary artery in an adolescent with complex congenital heart disease and right heart failure. This case brings to light the difficulties associated with loss of central venous access and the potential advantages of a direct cardiac approach to catheterization.
A 17-year old girl presented with right heart failure (RHF). She had a history of surgical repair of congenital pulmonary atresia with ventricular septal defect (PA-VSD) and discontinuous pulmonary arteries (PAs) for which unifocalisation was done and a right ventricle to pulmonary artery (RV-PA) conduit was placed along with VSD closure at age 3 years. At age 4 years, her right pulmonary artery (RPA) was noted to be atretic on a catheterization performed through the left internal jugular (IJ) vein, as both femoral veins and the right IJ were noted to be occluded. No attempt was made to recanalize the RPA during or following this procedure.
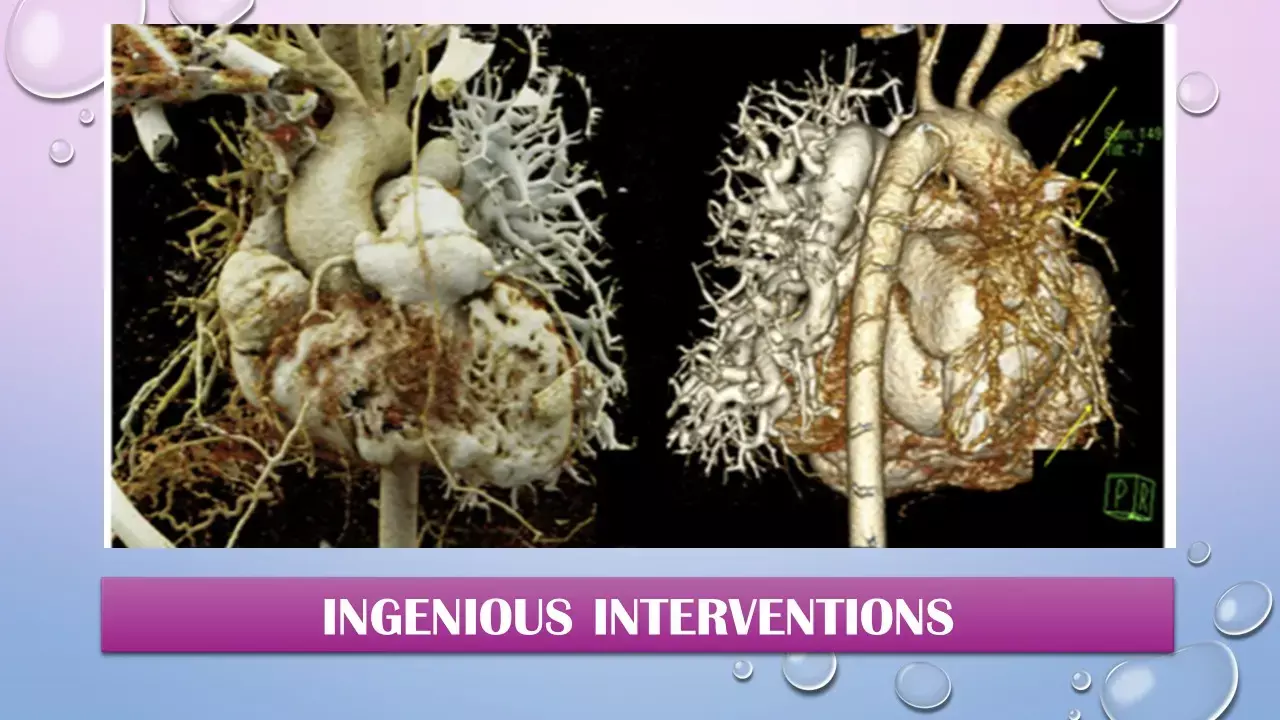
Over the next 13 years, the girl gradually developed symptoms of severe pulmonary artery hypertension with worsening exercise intolerance. Cardiac magnetic resonance (CMR) was performed when she was 17 years of age, which demonstrated severe RV dysfunction (RV ejection fraction of 17%) and dilation (end-diastolic volume of 288 cm/m2 ). Attempts were made to recanalize a densely atretic RPA, but the angles of approach made the intervention untenable.
The surgery team declined the possibility of any open surgery intervention, so a transthoracic direct cardiac access (DCA) was planned to recanalize the RPA. Using the Seldinger technique, a short guidewire was passed from a 21- gauge access needle into the RVOT and then to the distal left PA. The RPA was carefully recanalized using chronic total occlusion (CTO) hardware. The prehilar RPA was stented, and the bleeding from the conduit access site was occluded by Amplatzer duct occluder.
RPA stent redilation was done at a later staged procedure and further RPA rehabilitation 4 months later. At that time, her clinical symptoms of RHF had almost completely resolved. Her RV pressure was down to 75% systemic at repeat catheterization. The RPA stent was further dilated to 10-mm diameter. The right middle lobe PA branch was ultimately recanalized using the CTO wire technique and balloon angioplasty. Features of severe PAH improved drastically and later she underwent transcatheter pulmonary valve replacement to help reduce her RV volume, which eliminated her edema.
In children with congenital heart disease (CHD), there are only rare reports of DCA. Providing an additional parallel vascular bed surface area is an important strategy that can at times be used to relieve RV hypertension. In this case, the presence of advanced vascular disease in the left lung made recanalization of the RPA even more urgent. This case also highlights the fact that recanalization and revascularization following many years of complete occlusion can be achieved and that such revascularization can result in a meaningful redistribution of pulmonary blood flow. In this patient, at the latest evaluation, there was a 29% flow to the right lung. Hence, the interventionalist should be encouraged to consider recanalization of longstanding pulmonary artery atresia if RV hypertension or other indications are present.
Source : JACC case reports. J Am Coll Cardiol Case Rep. Dec 23, 2020. Epublished DOI: 10.1016/j.jaccas.2020.09.025
MBBS, MD , DM Cardiology
Dr Abhimanyu Uppal completed his M. B. B. S and M. D. in internal medicine from the SMS Medical College in Jaipur. He got selected for D. M. Cardiology course in the prestigious G. B. Pant Institute, New Delhi in 2017. After completing his D. M. Degree he continues to work as Post DM senior resident in G. B. pant hospital. He is actively involved in various research activities of the department and has assisted and performed a multitude of cardiac procedures under the guidance of esteemed faculty of this Institute. He can be contacted at editorial@medicaldialogues.in.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


