- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Acute Total Occlusion elevates Long-Term Risk of MACE in NSTEMI Patients undergoing PCI: Study
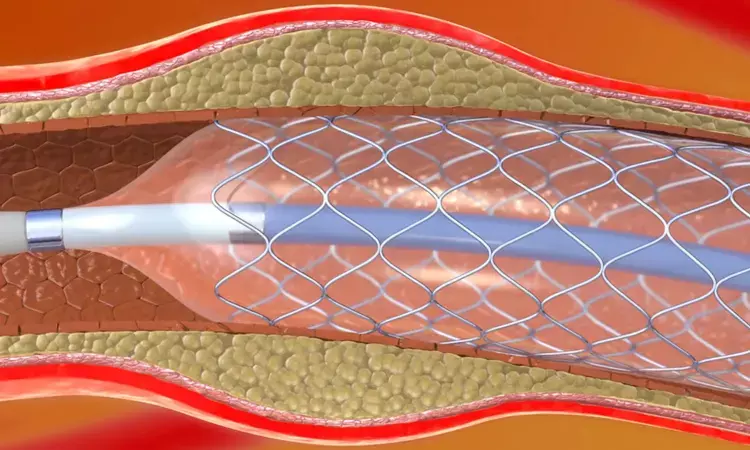
A new study published in The American Journal of Cardiology revealed acute total occlusion (ATO) in non-ST-segment elevation myocardial infarction (NSTEMI) patients undergoing PCI, which was most common in the left circumflex artery. ATO was associated with a 46% higher risk of major adverse cardiovascular events (MACE) over 3.6 years (aHR 1.46; p=0.002).
In a retrospective analysis of 1,128 NSTEMI patients who underwent coronary angiography this research was set determine the impact of vessel occlusion on clinical outcomes. The patients were divided into a group with total occlusion (TO) and other group with non-total occlusion (Non-TO). The study followed patients for a median of 3.6 years to track the occurrence of MACE, including all-cause death, non-fatal heart attack, non-fatal stroke, unplanned revascularization, and hospitalization for heart failure.
The analysis found that 286 patients (25.4%) had acute total occlusion, with the left circumflex artery being the most commonly affected vessel. These patients tended to have more severe clinical presentations and a higher burden of cardiovascular risk factors compared to those in the Non-TO group.
When outcomes were compared, thepatients in the TO group showed a 46% higher risk of MACE than those without complete blockage. The adjusted hazard ratio (aHR) was 1.46, with a 95% confidence interval (CI) of 1.16–1.83 and a p-value of 0.002, indicating a statistically significant difference. Total vessel blockage at the time of diagnosis was a strong predictor of poorer long-term outcomes.
While incorporating occlusion status into the well-known GRACE risk score, the predictive accuracy for MACE improved. This suggests that knowing whether the culprit artery is completely blocked could help clinicians more accurately identify high-risk patients and tailor treatment strategies accordingly.
A detailed breakdown of patient characteristics showed that those in the TO group had higher rates of cardiac enzyme elevation, lower left ventricular ejection fractions (indicating reduced heart pumping function), and more frequent multi-vessel disease. The rate of subsequent hospitalizations and revascularization procedures was also notably higher among these patients.
Overall, these findings highlighted that acute total occlusion in NSTEMI patients independently predicts worse cardiovascular outcomes, and integrating this parameter into existing risk models could enhance clinical decision-making and improve patient management in real-world settings.
Source:
Yu, Q., Wang, S., Zhao, Y., Zhao, Y., Zeng, J., Wang, Y., Fan, Z., Liu, F., & Liu, Z. (2025). Impact of acute total occlusion of the culprit vessel on prognosis and risk stratification in patients with non-ST-segment elevation myocardial infarction. The American Journal of Cardiology, 254, 139–146. https://doi.org/10.1016/j.amjcard.2025.07.042
Neuroscience Masters graduate
Jacinthlyn Sylvia, a Neuroscience Master's graduate from Chennai has worked extensively in deciphering the neurobiology of cognition and motor control in aging. She also has spread-out exposure to Neurosurgery from her Bachelor’s. She is currently involved in active Neuro-Oncology research. She is an upcoming neuroscientist with a fiery passion for writing. Her news cover at Medical Dialogues feature recent discoveries and updates from the healthcare and biomedical research fields. She can be reached at editorial@medicaldialogues.in
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


