- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Effectiveness of awake prone posture in respiratory failure by COVID-19 infection
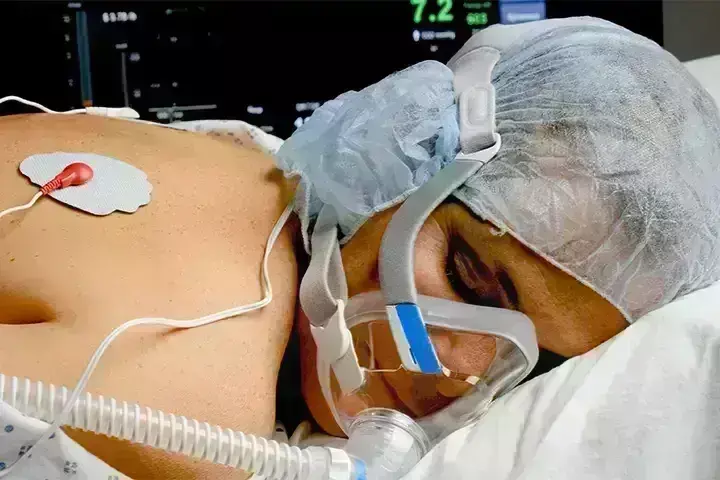
Due to increasing respiratory failure, a considerable number of individuals with COVID-19 need hospitalisation and oxygen treatment. The prevalence of intubation ranges between 15% and 85% and is a particular problem in places with the greatest death rates owing to extraordinary strain on healthcare systems. Prone placement is considered standard therapy for intubated patients with moderate to severe acute respiratory distress syndrome (ARDS), since it has the physiological advantage of increasing lung heterogeneity and aeration, which eventually results in increased survival.
Recently, authors published a multicenter open-label randomised controlled study evaluating the potential for APP to minimise the requirement for intubation and invasive ventilation in patients with COVID-19-induced acute hypoxemic respiratory failure when compared to conventional treatment (AHRF).
Researchers randomly allocated patients with COVID-19-induced acute hypoxemic respiratory failure (AHRF) who required high-flow nasal cannula (HFNC) oxygen to APP or conventional treatment in this multicenter randomised controlled study. The primary outcome measure was the rate of intubation at 28 days. Multiple regression analyses were used to determine the determinants of therapy success (survival without intubation).
Among the 430 patients randomly allocated, 216 received APP and 214 received conventional treatment. The APP group had a lower rate of intubation (30% vs 43%) and a shorter hospital stay (11 interquartile range [IQR, 9–14] vs 13 [IQR, 10–17] days, P = 0.001). A respiratory rate of 25 beats per minute at enrolment, an increase in ROX index > 1.25 after the first APP session, an APP duration of > 8 hours per day, and a drop in lung ultrasonography score 2 during the first 3 days were all related with therapeutic effectiveness for APP.
APP decreased the incidence of intubation and enhanced treatment effectiveness in individuals with COVID-19-induced AHRF treated with HFNC. A longer period of APP is linked with greater success, and the rise in ROX index and drop in lung ultrasonography score after APP may also assist select individuals who will benefit.
The results of this multicenter randomised controlled study demonstrated that APP was safe and significantly decreased intubation and hospital length of stay in patients with COVID-19-induced AHRF supported by HFNC, with a number-needed-to-treat of eight patients to prevent one intubation. More significantly, in-depth post hoc analyses identified indicators of APP effectiveness, including an APP duration > 8 h/day, a respiratory rate of 25 breaths/min before enrolment, and a favourable reaction to APP, as measured by an increase in the ROX index and lung ultrasonography score after APP.
Applying the advantages of prone posture to non-intubated patients is very difficult; in fact, only 6% and 27% of patients, respectively, attained the 16 h/day target in published trials.
These data imply that an APP duration of 8 hours per day is a feasible and useful goal for non-intubated patients.
In conclusion, as compared to standard treatment, APP decreased the incidence of intubation and duration of stay in patients with COVID-19-induced AHRF needing HFNC support. A longer daily duration of APP, a lower respiratory rate before to APP, and a good response to APP over the first three days were all related with a greater likelihood of treatment success. Our findings support the use of APP as a standard of care that should be started early and maintained for as long as feasible, with a minimum of 8 hours per day.
Reference –
Ibarra-Estrada, M., Li, J., Pavlov, I. et al. Factors for success of awake prone positioning in patients with COVID-19-induced acute hypoxemic respiratory failure: analysis of a randomized controlled trial. Crit Care 26, 84 (2022). https://doi.org/10.1186/s13054-022-03950-0
MBBS, MD (Anaesthesiology), FNB (Cardiac Anaesthesiology)
Dr Monish Raut is a practicing Cardiac Anesthesiologist. He completed his MBBS at Government Medical College, Nagpur, and pursued his MD in Anesthesiology at BJ Medical College, Pune. Further specializing in Cardiac Anesthesiology, Dr Raut earned his FNB in Cardiac Anesthesiology from Sir Ganga Ram Hospital, Delhi.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


