- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Rare Dual Diagnosis: Alport Syndrome and Immune Complex-Mediated MPGN Coexist in the Same Patient
Turkey: A recently reported case highlights the unusual coexistence of Alport syndrome and immune complex-mediated membranoproliferative glomerulonephritis (IC-MPGN) in the same patient—a rare dual glomerular pathology that complicates both diagnosis and management. The case highlights the need for timely renal biopsy and genetic evaluation in patients with progressive glomerular disease and a positive family history of renal involvement.
The case, published in BMC Nephrology by Dr. Seyda Gul Ozcan and colleagues from the Division of Nephrology, Cerrahpasa Medical Faculty, Istanbul University-Cerrahpasa, Turkey, describes a 42-year-old woman of Balkan origin who presented with persistent proteinuria and hematuria. Despite preserved kidney function at initial presentation, her renal parameters gradually worsened over the years. Family history was remarkable for kidney disease—her sister had undergone renal transplantation for focal segmental glomerulosclerosis, while her father had end-stage renal disease requiring dialysis.
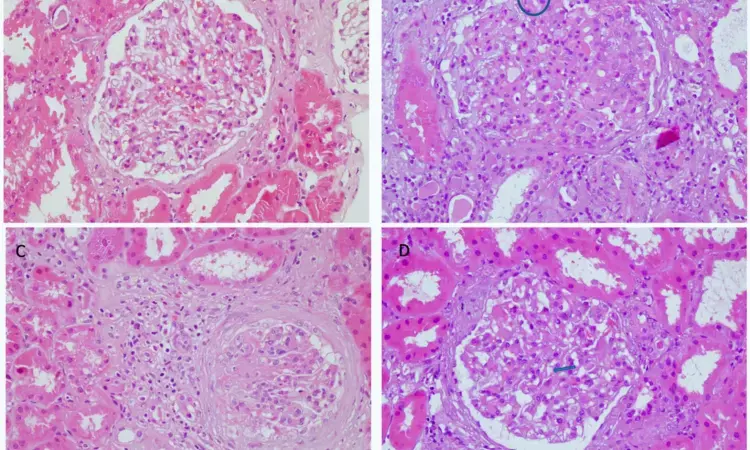
According to Dr. Ozcan and team, the patient initially declined a renal biopsy, leading to conservative management with ACE inhibitors. However, with progressive proteinuria and worsening creatinine levels, she eventually consented to a biopsy, which revealed mesangial expansion, glomerular basement membrane (GBM) thickening, endocapillary proliferation, and immune complex deposits positive for IgM, C3, and C1q—consistent with IC-MPGN. Complementary genetic testing identified a heterozygous COL4A5 mutation (c.1871G > A, p.Gly624Asp), confirming a diagnosis of X-linked Alport syndrome.
The patient also had extrarenal manifestations, including bilateral sensorineural hearing loss and mild hypertensive retinopathy, further supporting the Alport diagnosis. Immunosuppressive therapy with prednisolone and mycophenolate mofetil was initiated due to progressive disease, but had to be discontinued after the patient developed steroid-induced proximal myopathy. She is now being managed conservatively with renin–angiotensin–aldosterone system (RAAS) blockade and blood pressure control.
The authors highlighted that distinguishing between immune complex-mediated disease and nonspecific immune deposits in hereditary nephropathies can be challenging. While some previous reports have described immune complex-like staining in Alport syndrome, the biopsy findings in this patient fulfilled clear criteria for IC-MPGN, suggesting a true coexistence of the two conditions rather than passive deposition.
The report further notes that structural abnormalities in the GBM, as seen in Alport syndrome, may predispose patients to secondary immune complex deposition or unmask underlying complement dysregulation. However, such overlap remains extremely rare, with only a handful of cases reported in the literature.
“The case emphasizes the value of combining renal biopsy with genetic testing in patients with atypical clinical courses or a strong family history of kidney disease,” the authors concluded. They also pointed out that recognizing dual pathologies is crucial, as they may carry different prognostic and therapeutic implications, and treatment decisions must balance disease progression with the risks of therapy-related complications.
The case adds to the growing body of evidence that genetic kidney disorders may occasionally coexist with immune-mediated conditions, creating complex diagnostic and therapeutic scenarios. For clinicians, early suspicion, biopsy confirmation, and genetic testing remain critical tools in navigating such rare but clinically significant cases.
Reference:
Ozcan, S.G., Koc, E., Murt, A. et al. A rare case of dual glomerular pathology: Alport syndrome and immune complex-mediated MPGN. BMC Nephrol 26, 514 (2025). https://doi.org/10.1186/s12882-025-04400-z
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


