- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Rare case of Valproate induced Hyperammonemic encephalopathy
Dr Suhal Shah at Orange Regional Medical Center, Middletown, New York, USA, and colleagues have reported a case of Valproate induced hyperammonemic encephalopathy. The case has been published in the Journal of Medical Case Reports.
Valproic acid (VPA) is used with therapeutic plasma blood levels between 45 and 125 μg/ml to treat complex partial seizures, simple and complex absence seizures, migraines, bipolar mania, and schizoaffective disorders. The most commonly known side effects include sedation; dizziness; dose-dependent tremors; ataxia; headaches; and gastrointestinal side effects, including weight gain, abdominal pain, nausea, vomiting, diarrhea, constipation, and reduced appetite Hyperammonemic encephalopathy is a rare and serious adverse reaction to valproate. Although there is documentation of this reaction in previous reports, very little is still known about the exact mechanism of action. But rapid identification of this rare condition may lead to a favorable outcome.
According to the history, a 57-year-old Caucasian woman with a medical history of bipolar I disorder, previous psychiatric hospitalizations, opioid use disorder, benzodiazepine use disorder, and Crohn's disease as well as a family history of bipolar I disorder presented to the psychiatric emergency department with worsening anxiety and depressive symptoms. After a recent relationship breakup, she had begun experiencing multiple panic attacks and suicidal ideation, prompting her sister to call 911. She was admitted to the behavioral health unit of our hospital on an involuntary basis. Her admission laboratory test results were positive for benzodiazepines by urine toxicology.
During her intake interview after admission, she reported a decreased need for sleep, poor appetite, racing thoughts, increased energy level, panic attacks, anxiety, excessive spending, and feelings of helplessness. She denied any suicidal ideation, auditory/visual hallucinations, or paranoid thoughts. Her mental status examination revealed that she appeared to be her stated age, was casually dressed with good hygiene, and maintained good eye contact. She was cooperative during the interview process but provided tangential responses. Along with a constricted affect and anxious mood, she presented with rapid and pressured speech, increased distractibility, poor concentration, and lack of insight and judgment. She was diagnosed with bipolar I disorder, manic episode without psychotic features and benzodiazepine use disorder. The treatment team began her on a trial of VPA 500 mg twice daily by mouth for her mood, citalopram 20 mg by mouth once daily for her anxiety, propranolol 20 mg twice daily by mouth for panic attacks, and quetiapine 200 mg by mouth once nightly for sleep. Her dose of propranolol was increased to 30 mg twice daily by mouth. Her VPA level drawn on day 4 was within the therapeutic range, and she appeared less euphoric and less pressured. She denied experiencing any side effects from her medication, but on day 6, she was found to have a sudden onset of altered mental status, waxing and waning level of consciousness, confusion, lethargy, and ataxic gait. Upon physical examination, the patient was awake, alert, and oriented only to person. Her vital signs were stable with some fluctuations in blood pressure, likely secondary to her inconsistent compliance with propranolol. She was unable to follow commands or appropriately answer questions. To address any concerns regarding benzodiazepine withdrawal, which seemed to be less likely, given the absence of typical presentation (for example, tremors, restlessness, agitation, nausea, diaphoresis), the team initiated a detoxification protocol based on a symptom-triggered benzodiazepine treatment using Clinical Institute Withdrawal Assessment for Alcohol scale scoring.
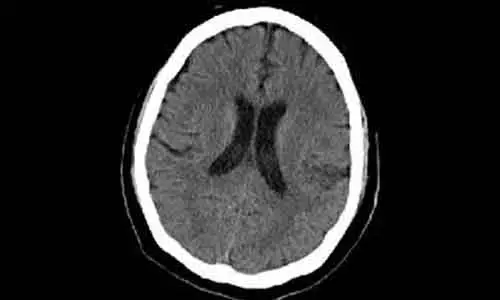
The patient did not score significantly on the detox protocol. The internal medicine and neurology services were consulted. The finding of computed tomography of the patient's head without contrast was negative, as were the results of repeat blood work and urinalysis. The patient's repeat urine toxicology screen was unchanged from admission. The only abnormality was her ammonia level of 58 μmol/L (normal range, 11–35 μmol/L). Her electrocardiogram (ECG) showed sinus tachycardia with a QTc interval of 502 milliseconds, which was attributed to citalopram administration. After the patient's ammonia level increased to 145 μmol/L 24 hours later, the treatment team suspected VHE, which led to discontinuation of all her medications. She was started on lactulose 20 g by mouth twice daily for 2 days, after which her ammonia level dropped to 32 μmol/L, and repeat ECG showed that her QTc interval was 454 milliseconds. Clinically, she returned to her baseline mentation. Given her reaction to VPA, she was instead started on a trial of lithium 900 mg once nightly and quetiapine 200 mg by mouth once nightly. Her lithium level after 4 days was 0.96 mmol/L, and she tolerated lithium well. By day 16, the patient was discharged with a level mood, no suicidal thoughts, and improved anxiety symptoms.
For further reference log on to: https://doi.org/10.1186/s13256-020-2343-x
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


