- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
How to manage retinal pigment tear in course of Anti VEGF therapy?
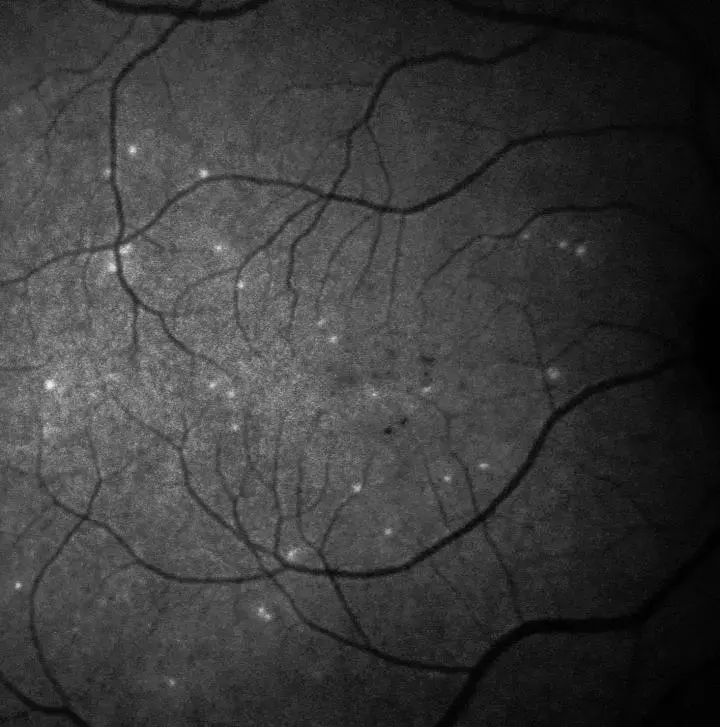 IMAGE: A PATIENT'S RETINA SHOWING HYPERFLUORESCENT SIGNALS - EACH WHITE SPOT IS A SINGLE 'SICK' RETINAL NERVE CELL. IMAGERY SUPPORTED BY DARC TECHNOLOGY USED IN THE PHASE II CLINICAL TRIAL. view more CREDIT: UCL/WESTERN EYE HOSPITAL
IMAGE: A PATIENT'S RETINA SHOWING HYPERFLUORESCENT SIGNALS - EACH WHITE SPOT IS A SINGLE 'SICK' RETINAL NERVE CELL. IMAGERY SUPPORTED BY DARC TECHNOLOGY USED IN THE PHASE II CLINICAL TRIAL. view more CREDIT: UCL/WESTERN EYE HOSPITALAge-related macular degeneration is a chronic degenerative condition that can lead to irreversible loss of vision. Neovascular AMD (nAMD) is characterized by growth of abnormal blood vessels beneath the macula (choroidal neovascularization [CNV]), and is usually treated with anti–vascular endothelial growth factor (VEGF) agents.
Retinal pigment epithelium tears are a relatively frequent occurrence in patients with nAMD and associated pigment epithelial detachment (PED), with reported incidence rates of 10% to 12% of eyes. In the longer term, visual acuity is frequently poor for these patients, particularly in the case of larger tears and if the foveal center is affected.
Although a range of retinal imaging modalities are recommended for the diagnosis and monitoring of RPE tear, there are currently no officially recognized guidelines, and a multimodal approach provides the most complete information. These modalities include color fundus photography, optical coherence tomography (OCT), fluorescein angiography (FA), OCT-angiography (OCT-A), near-infrared reflectance imaging, and fundus autofluorescence.
In the longer term, RPE tears are often associated with poor visual outcomes, particularly for tears involving the fovea and in cases where subretinal hemorrhage and scar formation occur. Therefore, the assessment of several prognostic markers is recommended in patients with PED considered at high risk of developing RPE tear during anti-VEGF treatment, although validation by prospective studies is necessary.
A literature search was conducted by Paul et al to review current evidence on the development, diagnosis, and management of retinal pigment epithelium (RPE) tear during anti–vascular endothelial growth factor (VEGF) therapy.
Three key recommendations were made based on existing literature and clinical experience:
1) Multimodal imaging with color fundus photography, optical coherence tomography, near-infrared reflectance imaging, fundus autofluorescence imaging, optical coherence tomography-angiography, and/or fluorescein angiography are recommended to diagnose RPE tear and assess risk factors. Retinal pigment epithelium tears can be graded by size and foveal involvement.
2) Patients at high risk of developing RPE tear should be monitored after each anti-VEGF injection. If risk factors worsen, it is not yet definitively known whether anti-VEGF administration should be more frequent, or alternatively stopped in such patients. Prospective research into high-risk characteristics is needed.
3) After RPE tear develops, anti-VEGF treatment should be continued in patients with active disease (as indicated by presence of intraretinal or subretinal fluid), although cessation of therapy should be considered in eyes with multilobular tears.
Overall, the incidence of RPE tear during anti-VEGF therapy in patients with PED is similar to that reported for untreated PED, with no clear evidence of differing risk according to use or type of anti-VEGF agent.
Although evidence to support the assumption that anti-VEGF treatment contributes to development of RPE tear is not definitive, some data suggest this link.
doi: 10.1097/IAE.0000000000003083
Dr Ishan Kataria has done his MBBS from Medical College Bijapur and MS in Ophthalmology from Dr Vasant Rao Pawar Medical College, Nasik. Post completing MD, he pursuid Anterior Segment Fellowship from Sankara Eye Hospital and worked as a competent phaco and anterior segment consultant surgeon in a trust hospital in Bathinda for 2 years.He is currently pursuing Fellowship in Vitreo-Retina at Dr Sohan Singh Eye hospital Amritsar and is actively involved in various research activities under the guidance of the faculty.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


