Doxycycline is a Broad spectrum Antibiotic used in the treatment of Various Bacterial infections
Cholera

Dose
300 mg single dose1
Scrub Typhus

Dose
100 mg BD for 7-15 days13
Malaria
Dose
100 mg BID on Day 1 followed by 100 mg OD for 6 days
Use in combination with quinine in areas of emerging quinine resistance11
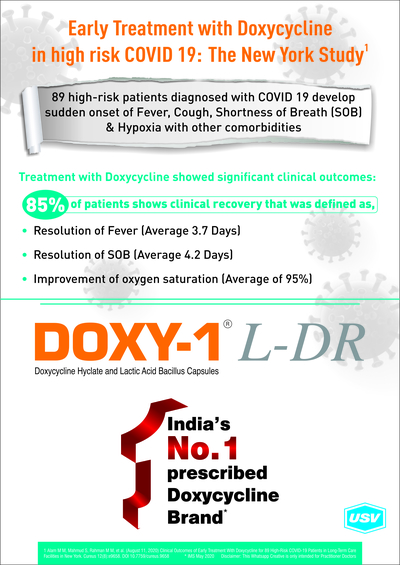
Viral Infections

Dose
200 mg on 1st day, then 100 mg OD12
Leptospirosis

Dose
100 mg BD for 7 days14
Pelvic inflammatory disease
Dose
100mg every 12 hours14
Sexually transmitted disease

Dose
100 mg twice daily for 7 days14
Infertility associated with STD
Dose
100mg BD for three weeks14
Vaginitis
Dose
100 mg every 12 hours for 7 days14
Pyrexia of unknown origin

Dose
100 mg BD as an empiric 1st antibiotic9
Skin and Soft tissue infection
Dose
200mg per os once daily
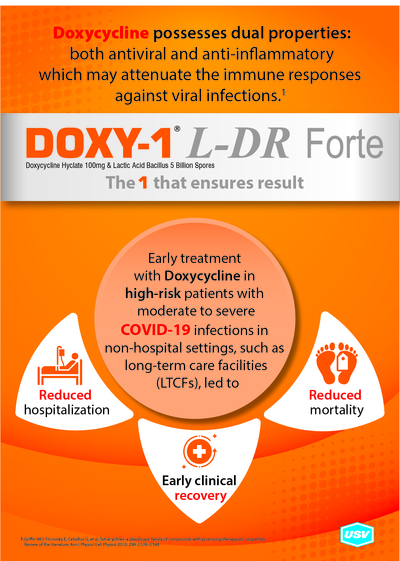
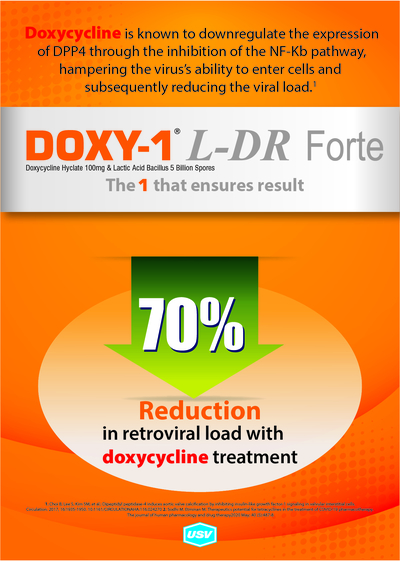
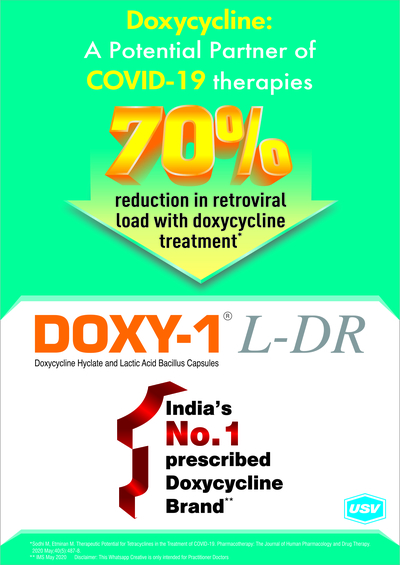
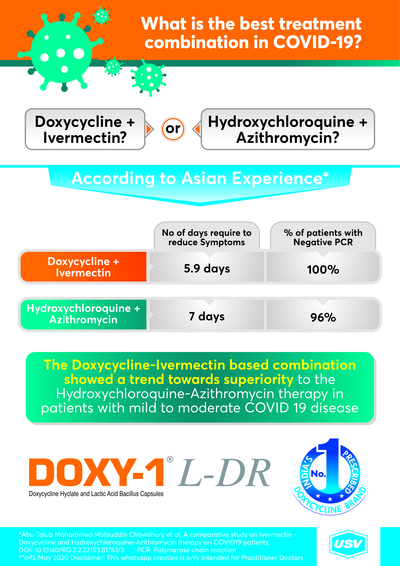
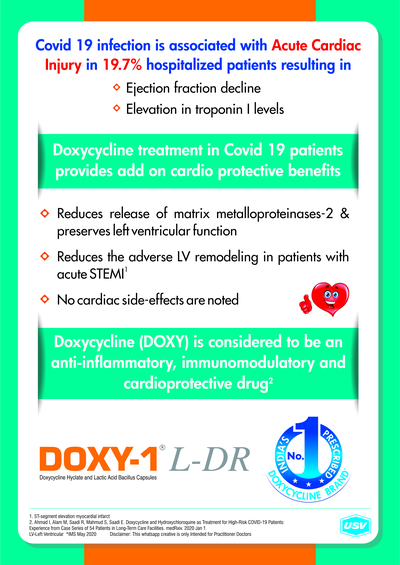
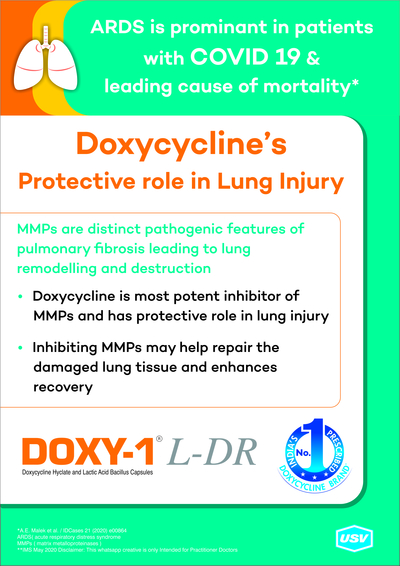
Doxycycline is a Potential Partner for Treatment of COVID-19 Infections
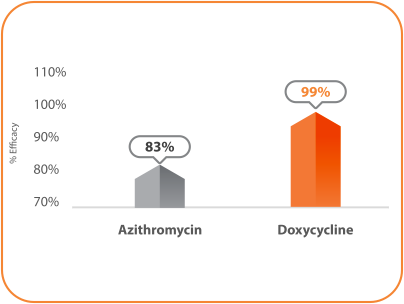
Antibiotic Response to Pediatric Scrub Typhus in South India: Is Clinical Failure to Azithromycin to be Worried?
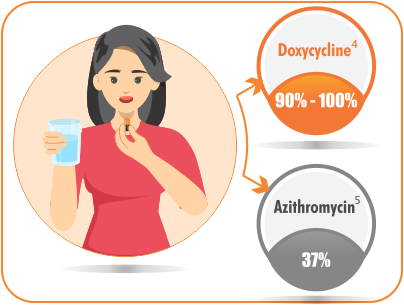
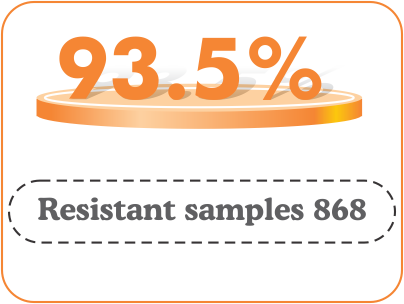
Background: Scrub typhus is typically associated with a rapid defervescence and clinical improvement within 48 h of initiation of appropriate antibiotics. But increasing reports of resistance to anti-rickettsial medications in scrub typhus are being reported in the literature.
Methods: This is a retrospective observational study of children up to the age of 14 years admitted between July 2017 and March 2020, to a private medical college hospital in southern part of India. The aim of this study was to compare the clinical response to antibiotic therapy with doxycycline and azithromycin in pediatric scrub typhus infection.
Results: One hundred thirty-eight children with scrub typhus infection were included for analysis. The median fever control time (h) was 12 (IQR ¼ 6–29) and 24 (IQR ¼ 10–52) with doxycycline and azithromycin respectively (p < 0.001*). Rapid fever control within 48 h was observed in 92% with doxycycline and in 74% with azithromycin (p < 0.001*). The clinical failure rate (defined by the necessity to change the antibiotics due to: (i) worsening of symptoms and signs of scrub typhus despite 48 h of antibiotics or (ii) persistence of fever and other symptoms of scrub typhus beyond 72 h), was significantly less with doxycycline (1%) compared with azithromycin (9.6%).
Conclusion: There has been a significant delayed clinical response to azithromycin in the treatment of scrub typhus in India, when compared to doxycycline. Hence it is preferable to use doxycycline as the first line of antibiotic for undifferentiated fever in scrub typhus endemic areas.
Lay summary: This retrospective study aims to compare the clinical response to doxycycline or azithromycin in the treatment of scrub typhus infection in children. The median fever control time, clinical failure rate and the proportion of children with rapid defervescence of fever within 48 h were significantly superior with doxycycline
Doxycycline Scores Over Azithromycin
- Methicillin-sensitive Staphylococcus aureus
- Methicillin-resistant Staphylococcus aureus
- Staphylococcus spp
- Streptococcus spp
- Streptococcus pneumoniae
- Enterococcus
Pelvic Inflammatory Disease and Clinical Utility of Doxycycline
Pelvic inflammatory disease (PID) is a common infection that can result in severe long-term morbidity, leading to chronic pelvic...
Therapeutic Indications:
Doxycycline capsules are used in the treatment of a variety of infections caused by susceptible strains of Gram-positive and Gram-negative bacteria and certain other micro-organisms.
Respiratory tract infections:Pneumonia and other lower respiratory tract infections due to susceptible strains of Streptococcus pneumoniae, Haemophilia influenzae, Klebsiella pneumoniae and other organisms. Mycoplasma pneumoniae pneumonia. Treatment of chronic bronchitis, Sinusitis.
Urinary tract infections:Infections caused by susceptible strains of Klebsiella species, Enterobacter species, Escherichia coli, Streptococcus faecalis and other organisms.
Sexually transmitted diseases:Infections due to Chlamydia trachomatis including uncomplicated urethral, endocervical or rectal infections. Non-gonococcal urethritis caused by Ureaplasma urealyticum (T-mycoplasma). Doxycline Capsules is also indicated in Chancroid granuloma inguinale and lymphogranuloma venereum., Doxycline Capsules is an alternative drug in the treatment of gonorrhoea and syphilis.
Skin infections:Acne vulgaris, when antibiotic therapy is considered necessary. Since Doxycycline is a member of the tetracycline series of antibiotics, it may be expected to be useful in the treatment of infections which respond to other tetracyclines, such as:
Ophthalmic infections:Due to susceptible strains of gonococci, staphylococci and Haemophilus influenzae. Trachoma, although, as judged by immunofluorescence, is not always eliminated. Inclusion conjunctivitis may be treated with oral Doxycycline alone or in combination with topical agents.
Rickettsial infections:Rocky Mountain spotted fever, typhus group, Q fever, Coxiella endocarditis and tick fevers.
Other infections:Psittacosis, brucellosis (in combination with streptomycin), cholera, bubonic plague, louse and tick-borne relapsing fever, tularaemia glanders, melioidosis, chloroquine-resistant falciparum malaria and acute intestinal amoebiasis (as an adjunct to amoebicides).
Doxycycline is an alternative drug in the treatment of leptospirosis, gas gangrene and tetanus.
Doxycycline is indicated for prophylaxis in the following conditions: Scrub typhus, travellers' diarrhoea (enterotoxigenic Escherichia coli), leptospirosis and malaria. Prophylaxis of malaria should be used in accordance to current guidelines, as resistance is an ever-changing problem.
Consideration should be given to official guidance on the appropriate use of antibacterial agents.
Doxycycline Dosage recommendations in specific infections:
50 mg daily with food or fluid for 6 - 12 weeks.
Sexually transmitted diseases:100 mg twice daily for 7 days is recommended in the following infections: uncomplicated gonococcal infections (except anorectal infections in men); uncomplicated urethral, endocervical or rectal infection caused by Chlamydia trachomatis; non-gonococcal urethritis caused by Ureaplasma urealyticum.
Acute epididymo-orchitis caused by Chlamydia trachomatis or Neisseria gonorrhoeae 100 mg twice daily for 10 days.
Primary and secondary syphilis:Non-pregnant penicillin-allergic patients who have primary or secondary syphilis can be treated with the following regimen: doxycycline 200 mg orally twice daily for two weeks, as an alternative to penicillin therapy.
Louse-borne and tick-borne relapsing fevers:A single dose of 100 mg or 200 mg according to severity.
Treatment Chloroquine-resistant falciparum malaria:200 mg daily for at least 7 days. Due to the potential severity of the infection, a rapid-acting schizonticide such as quinine should always be given in conjunction with Doxycycline; quinine dosage recommendations vary in different areas.
Prophylaxis of malaria:100mg daily in adults and children over the age of 12 years. Prophylaxis can begin 1-2 days before travel to malarial areas. It should be continued daily during travel in the malarial areas and for 4 weeks after the traveller leaves the malarial area. For current advice on geographical resistance patterns and appropriate chemoprophylaxis, current guidelines or the Malaria Reference Laboratory should be consulted, details of which can be found in the British National Formulary (BNF).
the prevention of scrub typhus:200 mg as a single dose.
For the prevention of travellers' diarrhea in adults:200 mg on the first day of travel (administered as a single dose or as 100 mg every 12 hours) followed by 100 mg daily throughout the stay in the area. Data on the use of the drug prophylactically are not available beyond 21 days.
For the prevention of leptospirosis:200 mg once each week throughout the stay in the area and 200 mg at the completion of the trip. Data on the use of the drug prophylactically are not available beyond 21 days.
Use in Elderly:Doxycycline may be prescribed in the usual dose with no special precautions. No dosage adjustment is necessary in the presence of renal impairment. Doxycycline Capsules may be preferred for the elderly since it is less likely to be associated with oesophageal irritation and ulceration.
Use in patients with Renal impairment:Studies to date have indicated that administration of Doxycycline at the usual recommended doses does not lead to excessive accumulation of the antibiotic in patients with renal impairment.
Method of administration
Doxycycline Capsules are for oral administration only.
The capsules should be swallowed with plenty of fluid in either the resting or standing position and well before going to bed for the night to reduce the likelihood of oesophageal irritation and ulceration.
If gastric irritation occurs, it is recommended that Doxycycline Capsules be given with food or milk.
Studies indicate that the absorption of doxycycline is not notably influenced by simultaneous ingestion of food or milk. Exceeding the recommended dosage may result in an increased incidence of side effects.
Therapy should be continued at least 24-48 hours after symptoms and fever have subsided. When used in streptococcal infections, therapy should be continued for 10 days to prevent the development of rheumatic fever or glomerulonephritis.
Doxycycline Contraindications-
Hypersensitivity to the active substance, any of the tetracyclines or to any of the excipients.
Doxycycline Pregnancy:
Doxycycline is contraindicated in pregnancy. It appears that the risks associated with the use of tetracyclines during pregnancy are predominantly due to effects on teeth and skeletal development.
Nursing mothers:Tetracyclines are excreted into milk and are therefore contra-indicated in nursing mothers.
Special warnings and precautions for use:
The use of drugs of the tetracycline class during tooth development (last half of pregnancy; infancy and childhood to the age of 8 years) may cause permanent discolouration of the teeth (yellow-grey-brown).
This adverse reaction is more common during long-term use of the drugs but has been observed following repeated short-term courses. Enamel hypoplasia has also been reported. Use doxycycline in paediatric patients aged younger than 8 years only when the potential benefits are expected to outweigh the risks in severe or life-threatening conditions (e.g. Rocky Mountain spotted fever), only when there are no adequate alternative therapies.
Although the risk of permanent teeth staining is rare in children aged 8 years to less than 12 years, the use of doxycycline should be carefully justified in situations where other drugs are not available, are not likely to be effective or are contraindicated.
Doxycycline Photosensitivity:Photosensitivity manifested by an exaggerated sunburn reaction has been observed in some individuals taking tetracyclines, including doxycycline. Patients likely to be exposed to direct sunlight or ultraviolet light should be advised that this reaction can occur with tetracycline drugs and treatment should be discontinued at the first evidence of skin erythema.
Doxycycline Use in patients with impaired hepatic function:Doxycycline should be administered with caution to patients with hepatic impairment or those receiving potentially hepatotoxic drugs. Abnormal hepatic function has been reported rarely and has been caused by both the oral and parenteral administration of tetracyclines, including doxycycline.
Doxycycline Use in patients with renal impairment:Excretion of doxycycline by the kidney is about 40%/ 72 hours in individuals with normal renal function. This percentage excretion may fall to a range as low as 1 - 5%/72 hours in individuals with severe renal insufficiency (creatinine clearance below 10 ml/min). Studies have shown no significant difference in the serum half-life of doxycycline in individuals with normal and severely impaired renal function. Haemodialysis does not alter the serum half-life of doxycycline. The anti-anabolic action of the tetracyclines may cause an increase in blood urea. Studies to date indicate that this anti-anabolic effect does not occur with the use of Doxycycline in patients with impaired renal function.
Serious Doxy skin reactions:Serious Doxy skin reactions, such as exfoliative dermatitis, erythema multiforme, Stevens-Johnson syndrome, toxic epidermal necrolysis, and drug reaction with eosinophilia and systemic symptoms (DRESS) have been reported in patients receiving doxycycline. If serious skin reactions occur, doxycycline should be discontinued immediately and appropriate therapy should be instituted.
Benign intracranial hypertension:Bulging fontanelles in infants have been reported in individuals receiving tetracyclines. Benign intracranial hypertension (pseudotumor cerebri) has been associated with the use of tetracyclines including doxycycline. Benign intracranial hypertension (pseudotumor cerebri) is usually transient, however cases of permanent visual loss secondary to benign intracranial hypertension (pseudotumor cerebri) have been reported with tetracyclines including doxycycline. If visual disturbance occurs during treatment, prompt ophthalmologic evaluation is warranted. Since intracranial pressure can remain elevated for weeks after drug cessation patients should be monitored until they stabilize. Concomitant use of isotretinoin or other systemic retinoids and doxycycline should be avoided because isotretinoin is also known to cause benign intracranial hypertension (pseudotumor cerebri).
Microbiological overgrowth:The use of antibiotics may occasionally result in the over-growth of non-susceptible organisms including Candida. If a resistant organism appears, the antibiotic should be discontinued and appropriate therapy instituted.
Pseudomembranous colitis has been reported with nearly all antibacterial agents, including doxycycline, and has ranged in severity from mild to life-threatening. It is important to consider this diagnosis in patients who present with diarrhoea subsequent to the administration of antibacterial agents.
Clostridium difficile associated diarrhoea (CDAD) has been reported with use of nearly all antibacterial agents, including doxycycline, and has ranged in severity from mild diarrhoea to fatal colitis. Treatment with antibacterial agents alters the normal flora of the colon leading to overgrowth of C. difficile.
C. difficile produces toxins A and B, which contribute to development of CDAD.
Hypertoxin producing strains of C. difficile cause increased morbidity and mortality, as these infections can be refractory to antimicrobial therapy and may require colectomy. CDAD should be considered in all patients who present with diarrhoea after antibiotic treatment. Careful medical history is necessary since CDAD has been reported to occur over two months after the administration of antibacterial agents.
Oesophagitis:Instances of oesophagitis and oesophageal ulcerations have been reported in patients receiving capsule and tablet forms of drugs in the tetracycline class, including doxycycline. Most of these patients took medications immediately before going to bed or with inadequate amounts of fluid.
Porphyria:There have been rare reports of porphyria in patients receiving tetracyclines.
Venereal disease:When treating venereal diseases, where co-existent syphilis is suspected, proper diagnostic procedures including dark-field examinations should be utilised. In all such cases monthly serological tests should be made for at least four months.
Beta-haemolytic streptococci Infections:Infections due to group A beta-haemolytic Streptococci should be treated for at least 10 days.
Myasthenia gravis:Due to a potential for weak neuromuscular blockade, care should be taken in administering tetracyclines to patients with myasthenia gravis. Systemic lupus erythematosus: Tetracyclines can cause exacerbation of systemic Lupus Erythematosus (SLE).
Methoxyflurane:Caution is advised in administering tetracyclines with methoxyflurane.
Jarisch-Herxheimer reaction:Some patients with spirochete infections may experience a Jarisch-Herxheimer reaction shortly after doxycycline treatment is started. Patients should be reassured that this is a usually self-limiting consequence of antibiotic treatment of spirochete infections.
Doxycycline Side Effects:
| System Organ Class | Common ≥ 1/100 to < 1/10 | Uncommon≥1/1000 to <1/100 | Rare≥1/10,000 to <1/1000 | Not known Cannot be estimated from the available data. |
|---|---|---|---|---|
| Infections and infestations | Vaginal infection | Candida Infection | ||
| Blood and lymphatic system disorders | Haemolytic anaemia, neutropenia, thrombocytopenia, eosinophilia | |||
| Immune system disorders | Hypersensitivity (including anaphylactic shock, anaphylactic reaction, anaphylactoid reaction, angioedema, exacerbation of systemic lupus erythematosus, pericarditis, serum sickness, Henoch-Schonlein purpura, hypotension, dyspnoea, tachycardia, peripheral oedema and urticaria) | Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS), Jarisch-Herxheimer reactionb | ||
| Endocrine | Brown-black microscopic | |||
| disorders | discolouration of thyroid glands | |||
| Metabolism and nutrition disorders | Porphyria, decreased appetite | |||
| Nervous system disorders | Headache | Anxiety, benign intracranial hypertension (pseudotumor cerebri)*, fontanelle bulging | ||
| Ear and labyrinth disorders | Tinnitus | |||
| Vascular disorders | Flushing | |||
| Gastrointestinal disorders | Nausea/vomiting | Dyspepsia (Heartburn/gastritis) | Pancreatitis, pseudomembranous colitis, Clostridium difficile colitis, oesophageal ulcer, oesophagitis, enterocolitis, inflammatory lesions (with monilial overgrowth) in the anogenital region, dysphagia, abdominal pain, diarrhoea, glossitis, stomatitis | tooth discolourationaa |
| Hepatobiliary disorders | Hepatic failure, hepatitis, hepatotoxicity, jaundice, hepatic function abnormal | |||
| Skin and subcutaneous tissue disorders | Photosensitivity reaction, rash including maculopapular and erythematous rashes | Toxic epidermal necrolysis, Stevens-Johnson syndrome, erythema multiforme, dermatitis exfoliative, photoonycholysis, skin hyperpigmentationcc | ||
| Musculoskeletal, connective tissue and bone disorders | Arthralgia, myalgia | |||
| Renal and urinary disorders | Blood urea increased |
* Symptoms included blurring of vision, scotomata and diplopia. Permanent visual loss has been reported.
a. Reversible and superficial discolouration of permanent teeth has been reported with the use of doxycycline but frequency cannot be estimated from available data.
b. in the setting of spirochete infections treated with doxycycline.
c. with chronic use of doxycycline.
Doxycycline Overdose
Acute overdosage with antibiotics is rare. In the event of overdosage discontinue medication. Gastric lavage plus appropriate supportive treatment is indicated.
Dialysis does not alter serum half-life and thus would not be of benefit in treating cases of overdosage.
Doxycycline Pharmacological properties
Doxycycline is primarily a bacteriostatic and is believed to exert its antimicrobial effect by the inhibition of protein synthesis.
Doxycycline is clinically effective in the treatment of a variety of infections caused by a wide range of gram-negative and gram-positive bacteria, as well as certain other micro-organisms.
Pharmacokinetic properties
Tetracyclines are readily absorbed and are bound to plasma proteins in varying degrees. They are concentrated by the liver in the bile and excreted in the urine and faeces at high concentrations and in a biologically active form. Doxycycline is virtually completely absorbed after oral administration. Studies reported to date indicate that the absorption of doxycycline, unlike certain other tetracyclines, is not notably influenced by the ingestion of food or milk. Following a 200 mg dose, normal adult volunteers averaged peak serum levels of 2.6 micrograms/ml of doxycycline at 2 hours decreasing to 1.45 micrograms/ml at 24 hours. Doxycycline has a high degree of lipid solubility and a low affinity for calcium. It is highly stable in normal human serum. Doxycycline will not degrade into an epianhydro form.
Pharmaceutical Composition:
Microcrystalline Cellulose,
Purified Talc,
Magnesium Stearate,
Colloidal Silicon Dioxide,
Sodium Lauryl Sulphate,
Titanium Dioxide (E171),
Indigo Carmine (E132),
Erythrosine (E127),
Gelatin.