- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Antibiotics in Prosthetic valve endocarditis: AIIMS Guidelines
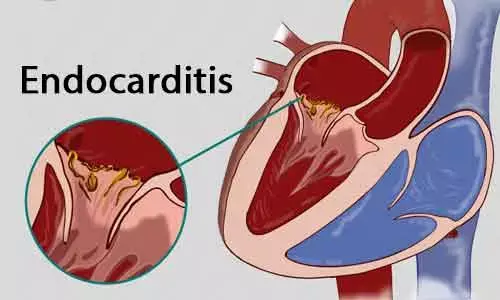
All India Institute of Medical Sciences, Delhi has released AIIMS Antibiotics Policy which has been prepared by the Department of Medicine with Multidisciplinary collaboration. The guidance for Infections pertaining to cardiology includes Prosthetic valve endocarditis the salient features of which are hereunder.
Prosthetic valve endocarditis (PVE): Traditionally, PVE has been classified as early, intermediate or late depending on the onset of symptoms of endocarditis following valve replacement surgery.
Early-onset PVE (within 60 days of surgery)- healthcare-acquired infections - Staphylococcus aureus commonest
Intermediate-onset PVE- 60 to 365 days- mix of healthcare- and community-acquired infections- coagulase-negative Staphylococcus (CONS) commonest
Late-onset PVE- more than 1 year - resemble native valve endocarditis (NVE)-S. aureus and CoNS
Indian studies have also shown predominance of gram positive cocci infections followed by non-HACEK gram negative bacilli in IE. A study from Hyderabad showed that Staphylococcus aureus constitutes around 30% of PVE cases. In this study methicillin resistant coagulase negative Staphylococcus spp.(MRCONS) infection constituted around 36% of culture positive PVE. Remaining 30 % was caused by non-HACEK gram negative bacilli.
When to suspect: -
Prosthetic valve endocarditis should be suspected in any patient with unexplained fever, night sweats, or signs of systemic illness after valve replacement surgery.
How to confirm –
Blood cultures should be obtained before initiation of antibiotic therapy. In critically ill patients, a minimum of three cultures from different venipuncture sites should be drawn over one hour before starting empiric therapy. In non–critically ill patients in whom endocarditis is suspected, therapy may be delayed until the results of blood cultures and echocardiography are available. Obtaining more than three blood cultures typically yields only minimal additional diagnostic information.
Baseline electrocardiography should be performed in patients with infective endocarditis so that new cardiac manifestations can be recognized early (e.g., extension of valvular disease into the conduction system, ischemia secondary to emboli to the coronary circulation). Echocardiography should be performed to identify valvular abnormalities in all patients in whom there is moderate or high suspicion of endocarditis. Transthoracic echocardiography is usually the initial imaging modality but has a modest sensitivity only. However, transesophageal echocardiography may be necessary in some patients, such as those with staphylococcus bacteremia, limited transthoracic windows because of obesity or mechanical ventilation, a prosthetic valve that renders visualization difficult secondary to shadowing, a history of endocarditis, or a structural valve abnormality.
a. Empiric:
Ceftriaxone 2gm iv OD plus Gentamicin 80 mg TDS plus Vancomycin 1g BD plus Rifampicin 300mg TDS
-Total duration at least 6 weeks
-Rifampicin to be added after 3 days
-In beta lacatam allergy- Inj Vancomycin 1g IV BD instead of beta-lactams
-Carbapenem can be used in place of ceftriaxone in suspicion of Gram negative sepsis
-Vancomycin can be replaced with Teicoplanin IV 10mg/kg loading BD X 3 doses, then 10mg/kg IV OD
b. Penicillin-susceptible Streptococci:
Preferred: Ampicillin 2gm Six times daily
Alternative: Ceftriaxone 2 g IV OD
-In beta lacatam allergy- Inj Vancomycin 1g IV BD instead of beta-lactams
-Amoxicillin 100-200 mg/kg/day in four to six divided doses can be used instead of ampicillin
-Note: Minimum duration for viridians group of streptococci is 2wks (depending on clinical response)
c. Penicillin resistant Streprococci:
Preferred: Ampicillin 2gm IV Six times daily plus Gentamicin 240 mg IV OD
Alternative: Ceftriaxone 2 g IV OD Plus Gentamicin 240 mg IV OD
Note: Gentamicin to be given only for first two weeks
d. MSSA:
Preferred: Inj Cefazolin 2gm iv TDS plus Rifampicin 300mg TDS plus Gentamicin 80mg TDS
-In beta lacatam allergy- Inj Vancomycin 1g IV BD instead of beta-lactams
-Gentamicin only for 1st 2 weeks
e. MRSA:
Preferred: Vancomycin 1g IV BD plus Rifampicin 300mg TDS plus Gentamicin 80mg TDS
- Gentamicin only for 1st 2 weeks
f. Enterococcus:
Ampicillin and gentamicin susceptible:
Preferred: Ampicillin + gentamicin (80 mg IV q8h)
Alternative: Ampicillin 2gm IV six times daily plus Ceftriaxone 2 g IV BD
Penicillin susceptible and high-level gentamicin resistant (HLAR):
Preferred: Ampicillin 2gm IV six times daily plus Ceftriaxone 2 g IV BD
Resistance to penicillin but Vancomycin- and Aminoglycoside-Susceptible Penicillin-Resistant
Preferred: Vancomycin 1g BD Plus Gentamicin 80 mg TDS
Alternative: Daptomycin 10-12 mg/kg OD or Teicoplanin 10 mg/kg iv 12 hrly 3-doses f/b iv OD can be used instead of vancomycin
Resistant to Penicillin, Aminoglycosides, and Vancomycin:
Preferred: Linezolid 600 mg IV BD
Alternative: Daptomycin 10–12 mg/kg OD
g. Fungal
Preferred:
-Liposomal Amphotericin B 3-5 mg/kg IV OD with or without Flucytosine 25mg/kg QID orally
-Step down to Fluconazole 400-800 mg/day once blood culture sterile and organism sensitive to Fluconazole
Alternative: Caspofungin 150 mg IV OD or Micafungin 150 mg IV OD or Anidulafungin 200mg IV OD
Remarks:
-Surgical excision is recommended for fungal endocarditis.
-Long term suppression with fluconazole 400 to 800 mg/day.
-If fluconazole resistant, can use voriconazole or Posaconazole
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


