- Home
- Medical news & Guidelines
- Anesthesiology
- Cardiology and CTVS
- Critical Care
- Dentistry
- Dermatology
- Diabetes and Endocrinology
- ENT
- Gastroenterology
- Medicine
- Nephrology
- Neurology
- Obstretics-Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Pediatrics-Neonatology
- Psychiatry
- Pulmonology
- Radiology
- Surgery
- Urology
- Laboratory Medicine
- Diet
- Nursing
- Paramedical
- Physiotherapy
- Health news
- Fact Check
- Bone Health Fact Check
- Brain Health Fact Check
- Cancer Related Fact Check
- Child Care Fact Check
- Dental and oral health fact check
- Diabetes and metabolic health fact check
- Diet and Nutrition Fact Check
- Eye and ENT Care Fact Check
- Fitness fact check
- Gut health fact check
- Heart health fact check
- Kidney health fact check
- Medical education fact check
- Men's health fact check
- Respiratory fact check
- Skin and hair care fact check
- Vaccine and Immunization fact check
- Women's health fact check
- AYUSH
- State News
- Andaman and Nicobar Islands
- Andhra Pradesh
- Arunachal Pradesh
- Assam
- Bihar
- Chandigarh
- Chattisgarh
- Dadra and Nagar Haveli
- Daman and Diu
- Delhi
- Goa
- Gujarat
- Haryana
- Himachal Pradesh
- Jammu & Kashmir
- Jharkhand
- Karnataka
- Kerala
- Ladakh
- Lakshadweep
- Madhya Pradesh
- Maharashtra
- Manipur
- Meghalaya
- Mizoram
- Nagaland
- Odisha
- Puducherry
- Punjab
- Rajasthan
- Sikkim
- Tamil Nadu
- Telangana
- Tripura
- Uttar Pradesh
- Uttrakhand
- West Bengal
- Medical Education
- Industry
Prasugrel superior to ticagrelor for ACS patients who underwent PCI: JAMA
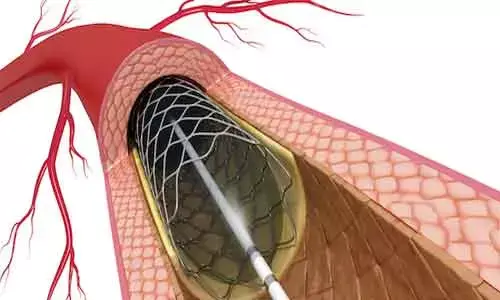
Germany: A prespecified subgroup analysis of a randomized clinical trial revealed that among patients with acute coronary syndrome (ACS) who underwent percutaneous coronary intervention (PCI), there was a lesser frequency of all-cause death, myocardial infarction when treated with prasugrel compared with ticagrelor.
The findings of this study are published in the journal JAMA Cardiology.
Ticagrelor is a platelet inhibitor known to reduce deaths in patients with acute coronary syndrome ACS or a history of myocardial infarction (MI). It is unclear whether ticagrelor or prasugrel hydrochloride is superior for patients with ACS treated with PCI. J. J. Coughlan, Deutsches Herzzentrum München, Technische Universität München, Munich, Germany, and colleagues aimed to assess the safety and efficacy of ticagrelor vs prasugrel for patients with ACS treated with PCI.
The study was a prespecified analysis performed of a post-randomization subgroup of 3377 patients who presented with ACS and were treated with PCI in the investigator-initiated, multicenter study conducted from September 1, 2013, to February 28, 2018. Statistical analysis was performed from September 1, 2020, to January 30, 2021. Analysis was performed according to the intention-to-treat principle. Patients were randomly assigned to a ticagrelor-based or prasugrel-based strategy. This analysis focused on the subgroup of patients who underwent PCI that was formed after randomization. The primary endpoint was a composite consisting of all-cause death, myocardial infarction, or stroke at 12 months. The safety endpoint was Bleeding Academic Research Consortium (BARC) type 3 to 5 bleeding.
The ticagrelor group comprised of 1676 patients (1323 men [78.9%]; mean age, 64.4 years), and the prasugrel group comprised 1701 patients (1341 men [78.8%]; mean age, 64.7 years).
The results of the study were:
• The primary endpoint occurred for 162 patients (9.8%) in the ticagrelor group and 120 patients (7.1%) in the prasugrel group (hazard ratio [HR], 1.41).
• Myocardial infarction was seen in 88 patients (5.3%) in the ticagrelor group compared with 55 patients (3.8%) in the prasugrel group (HR, 1.67).
• The safety endpoint, BARC type 3 to 5 bleeding, occurred in 84 of 1672 patients (5.3%) in the ticagrelor group and 78 of 1680 patients (4.9%) in the prasugrel group (HR; 1.10).
Dr. Coughlan and team conveyed that among patients presenting with ACS who were treated with PCI, the incidence of the primary composite endpoint occurred less frequently for patients who received prasugrel compared with those who received ticagrelor. However, because these observations were based on a post-randomization subgroup, they suggested these findings should be regarded as hypothesis-generating, and dedicated randomized clinical trials may be warranted to confirm these findings.
Reference:
Coughlan JJ, Aytekin A, Lahu S, et al. Ticagrelor or Prasugrel for Patients With Acute Coronary Syndrome Treated With Percutaneous Coronary Intervention: A Prespecified Subgroup Analysis of a Randomized Clinical Trial. JAMA Cardiol. 2021;6(10):1121–1129. doi:10.1001/jamacardio.2021.2228
Medical Dialogues consists of a team of passionate medical/scientific writers, led by doctors and healthcare researchers. Our team efforts to bring you updated and timely news about the important happenings of the medical and healthcare sector. Our editorial team can be reached at editorial@medicaldialogues.in.
Dr Kamal Kant Kohli-MBBS, DTCD- a chest specialist with more than 30 years of practice and a flair for writing clinical articles, Dr Kamal Kant Kohli joined Medical Dialogues as a Chief Editor of Medical News. Besides writing articles, as an editor, he proofreads and verifies all the medical content published on Medical Dialogues including those coming from journals, studies,medical conferences,guidelines etc. Email: drkohli@medicaldialogues.in. Contact no. 011-43720751


